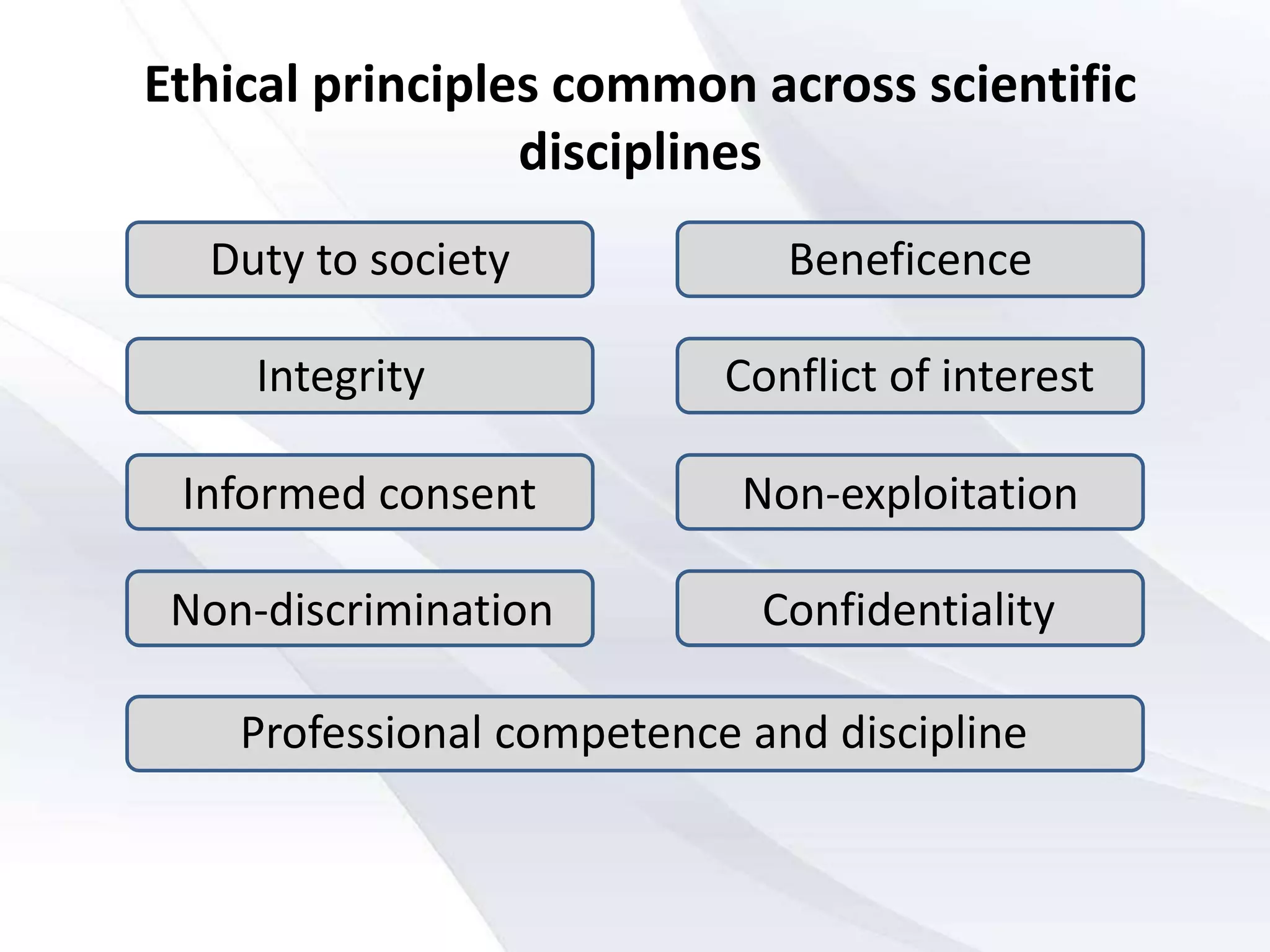
This document discusses ethical issues in scientific research involving human subjects. It outlines several key principles of research ethics including informed consent, minimizing harm, protecting privacy and confidentiality, ensuring justice and beneficence, and maintaining integrity. International codes like the Nuremberg Code, Helsinki Declaration, and Belmont Report established foundational ethical standards. Indian guidelines also adhere to strict ethical protocols for research involving human participants. Institutional ethics committees play an important role in reviewing research proposals and protocols to ensure compliance with ethical standards.