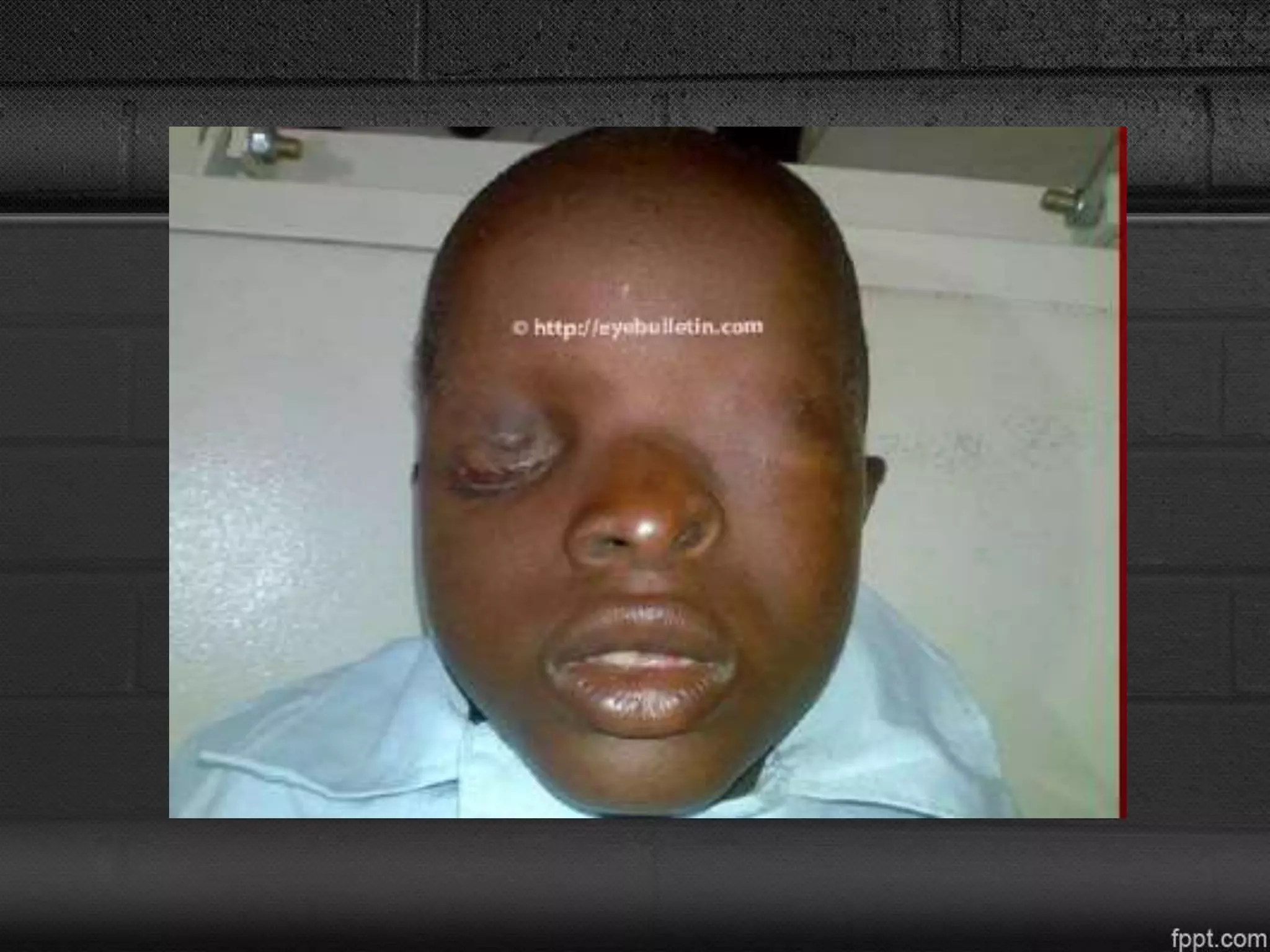
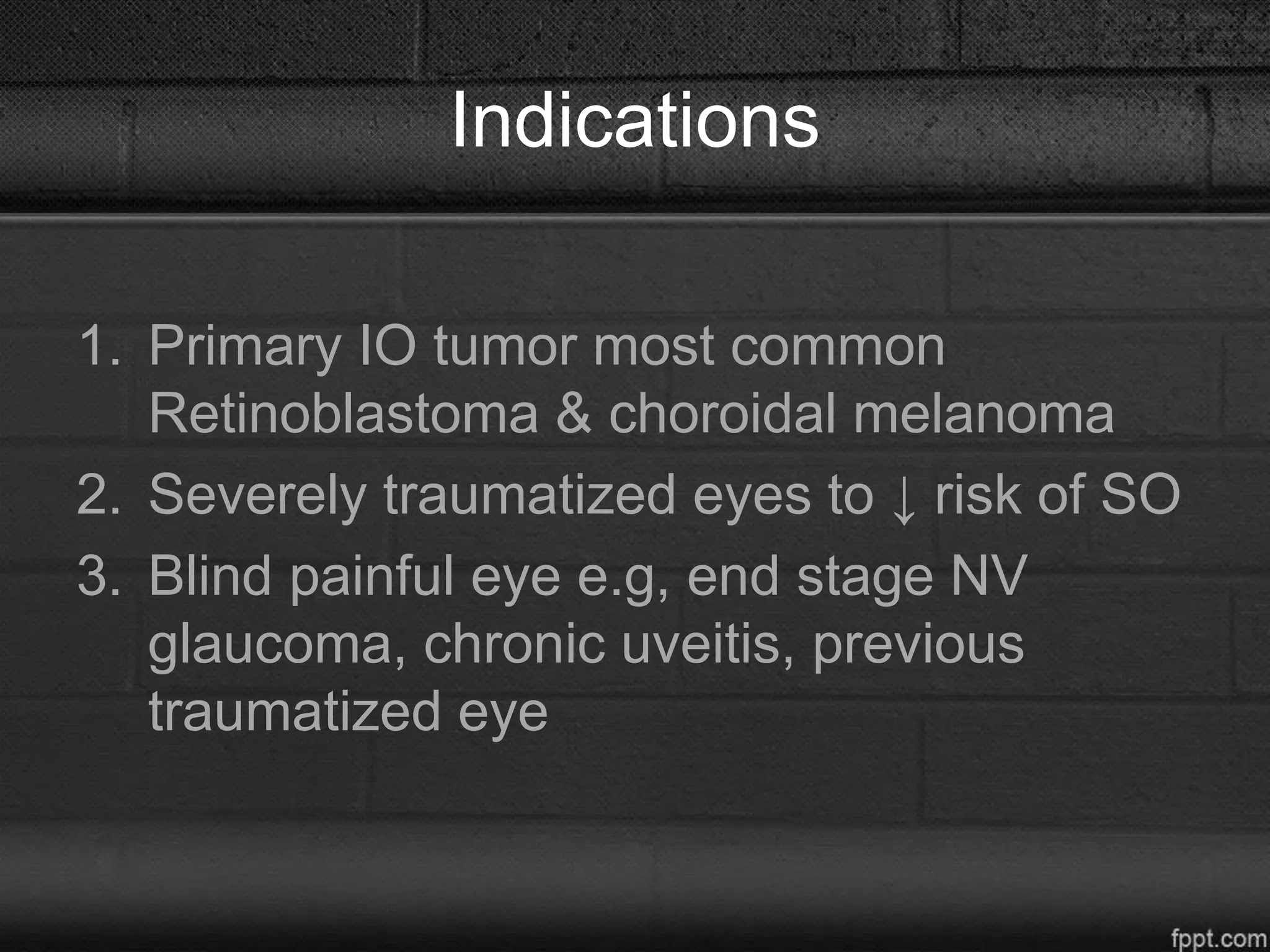
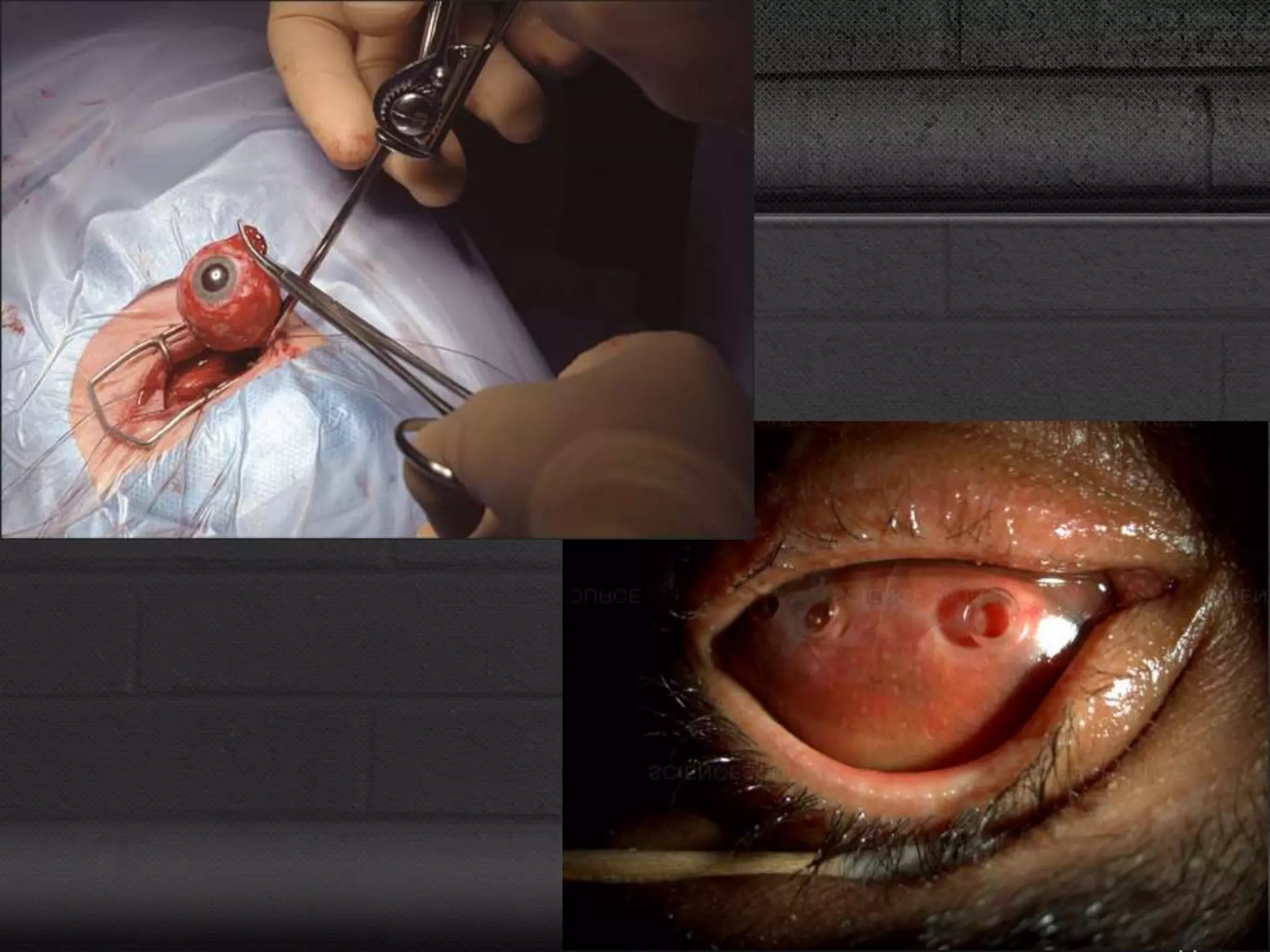
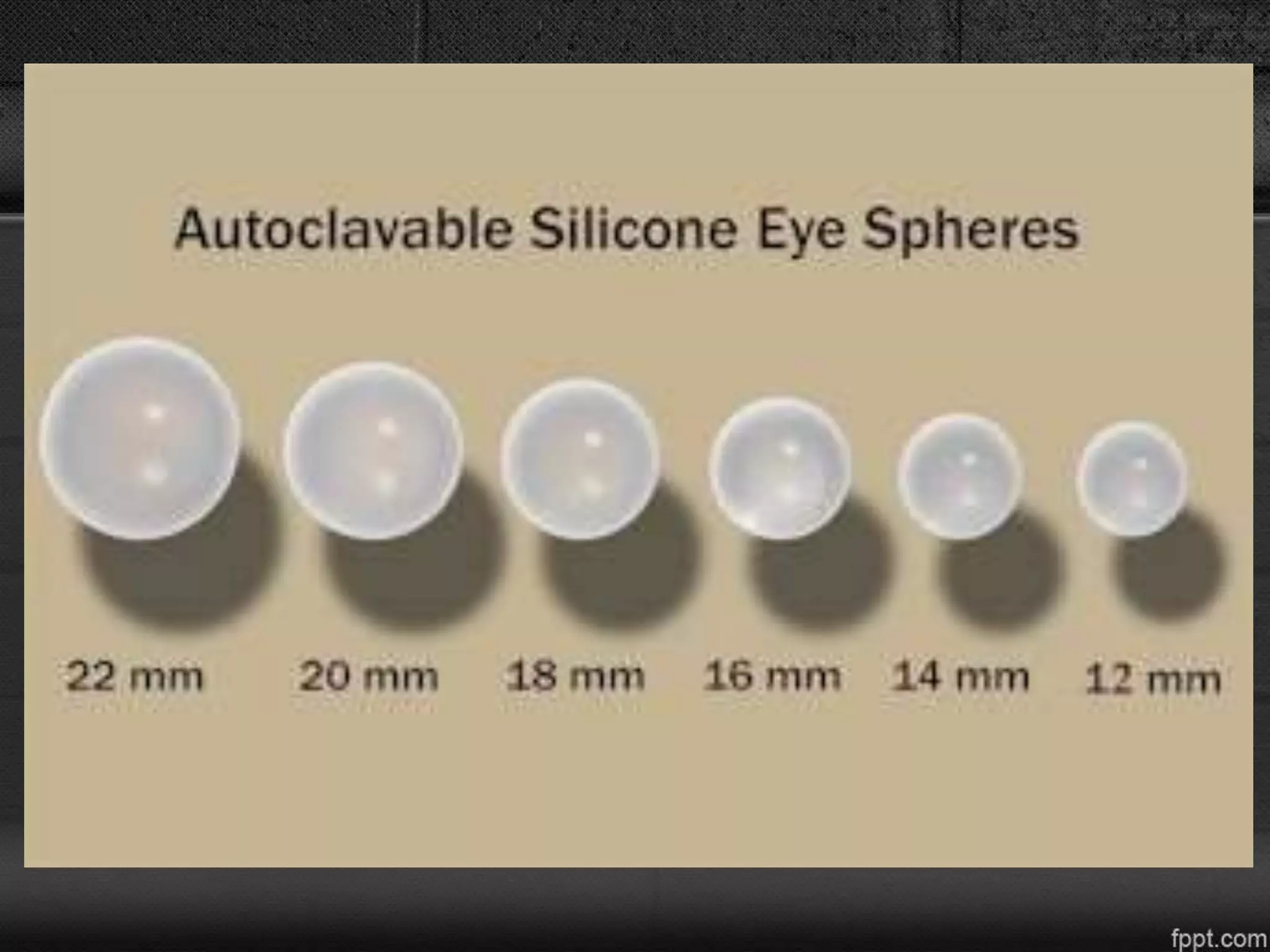
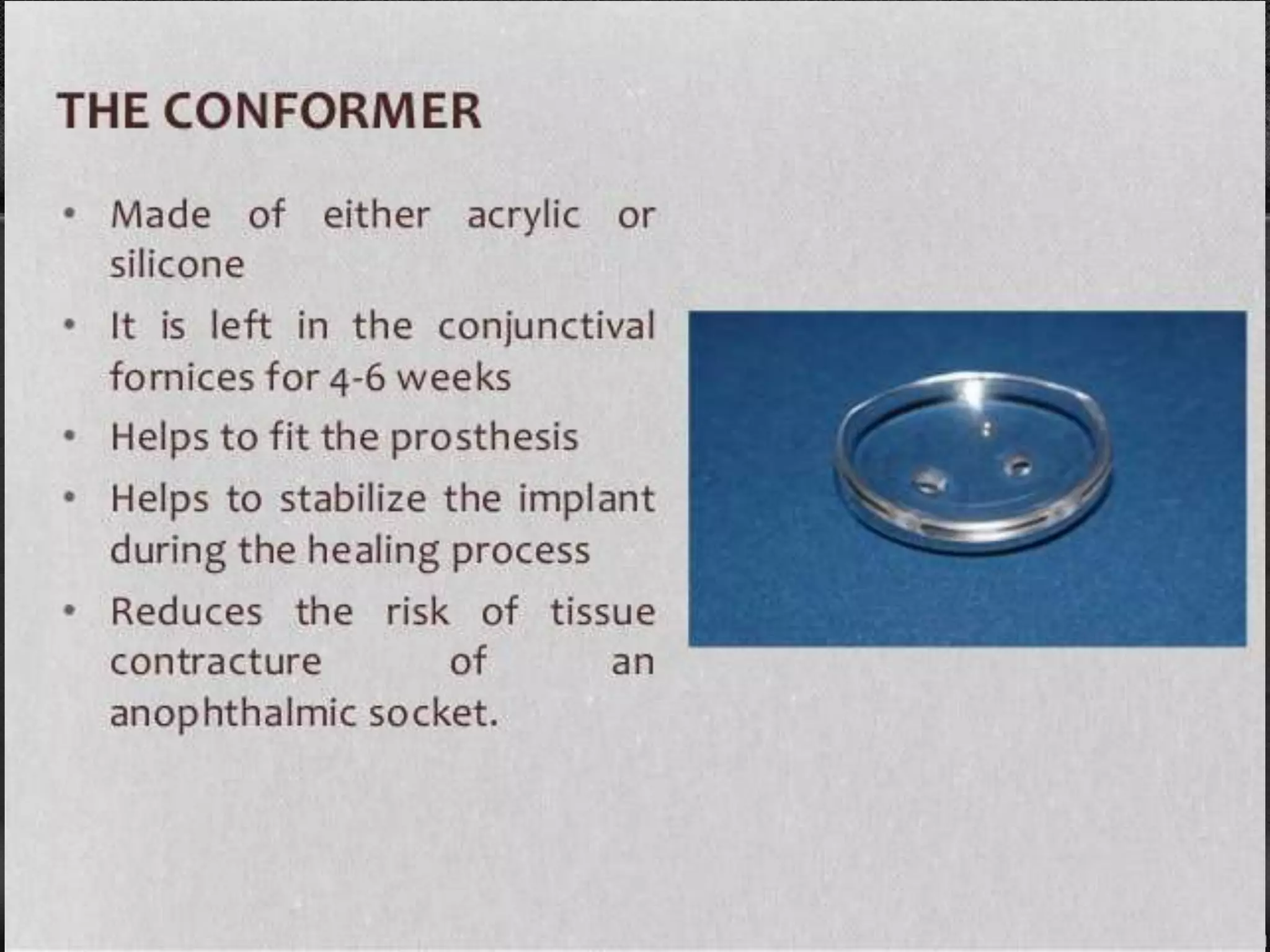
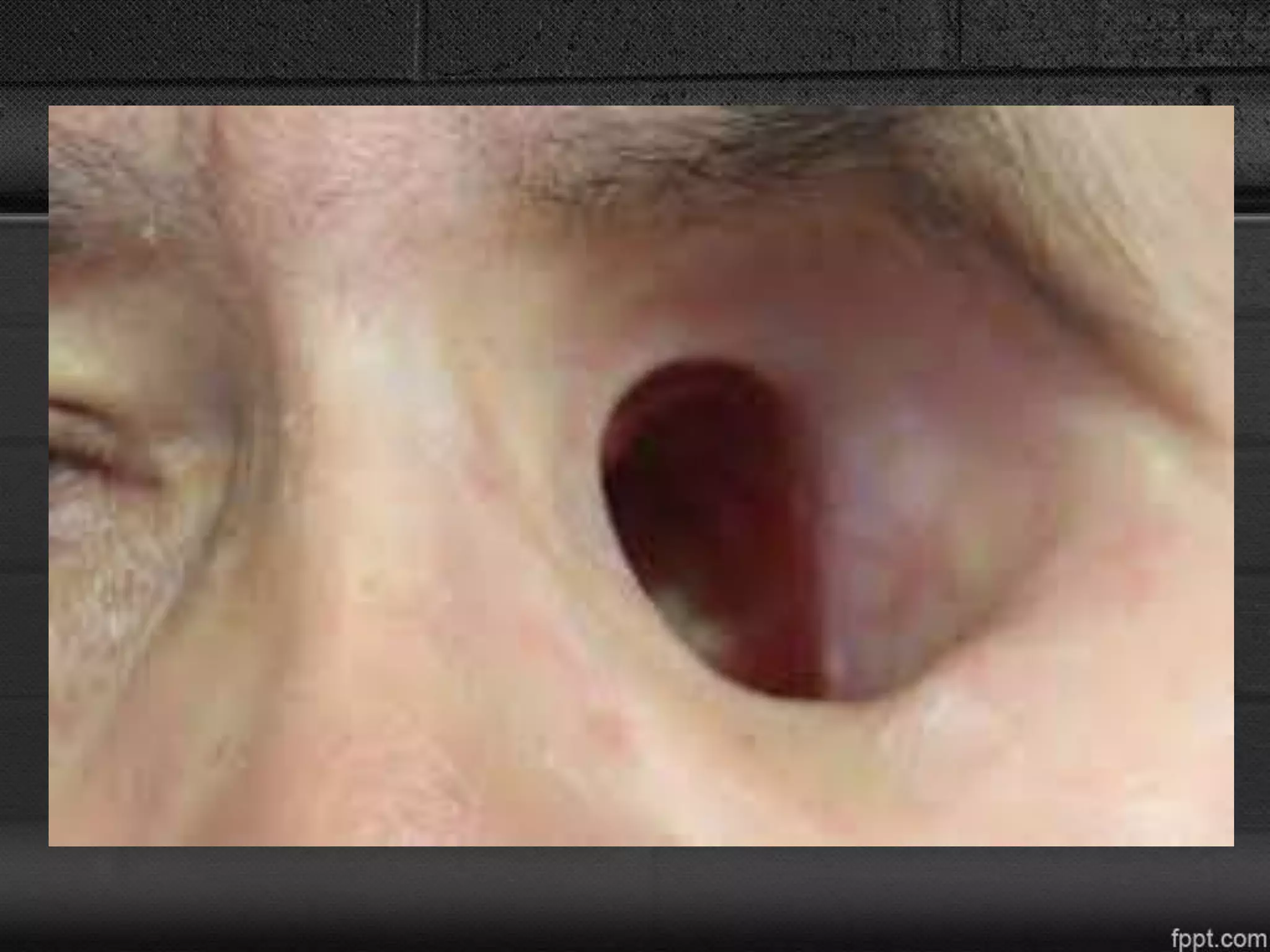
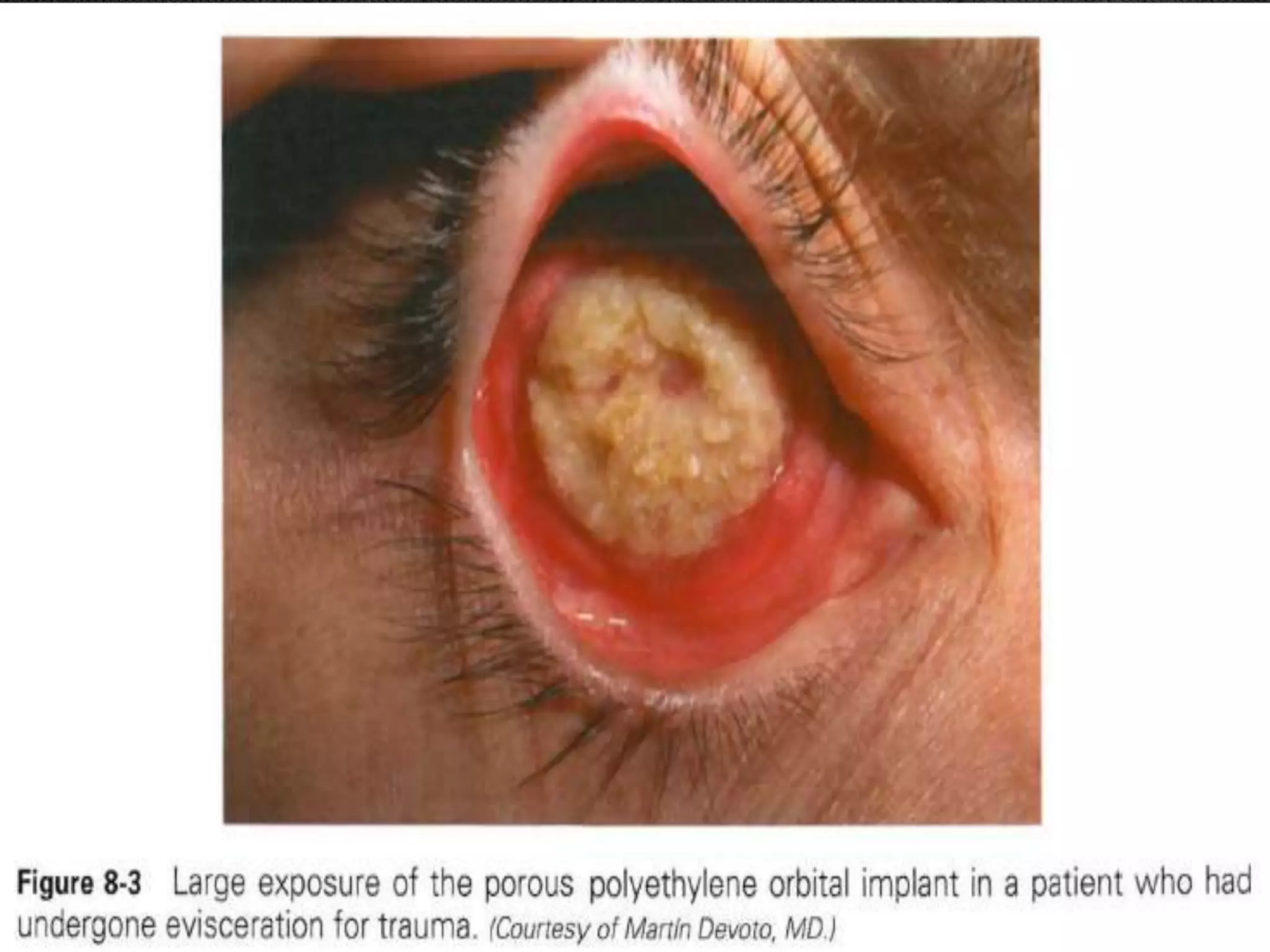
This document discusses the anatomy and management of the anophthalmic socket. It begins by defining an anophthalmic socket as an orbit lacking an eye globe, usually due to enucleation. True anophthalmia can be congenital or acquired. The most common causes of acquired anophthalmia are enucleation, exenteration, or evisceration performed to treat painful, blind eyes or remove tumors. The document outlines techniques for each procedure and discusses complications that can arise like socket contracture and management strategies like grafting. It emphasizes the importance of socket maintenance with conformers and prosthetics to prevent complications. In summary, this document provides an overview of anophthalmic socket anatomy,