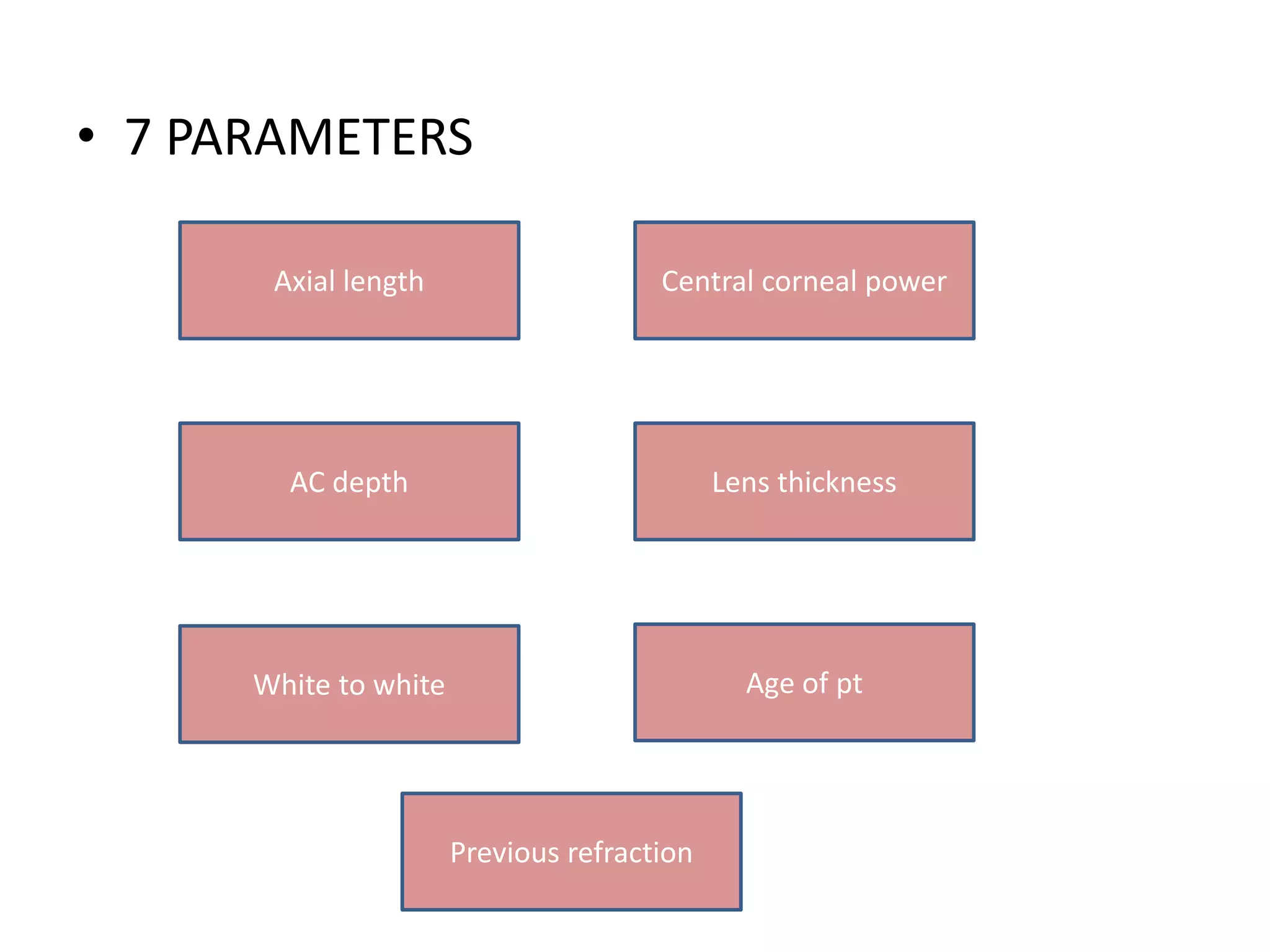
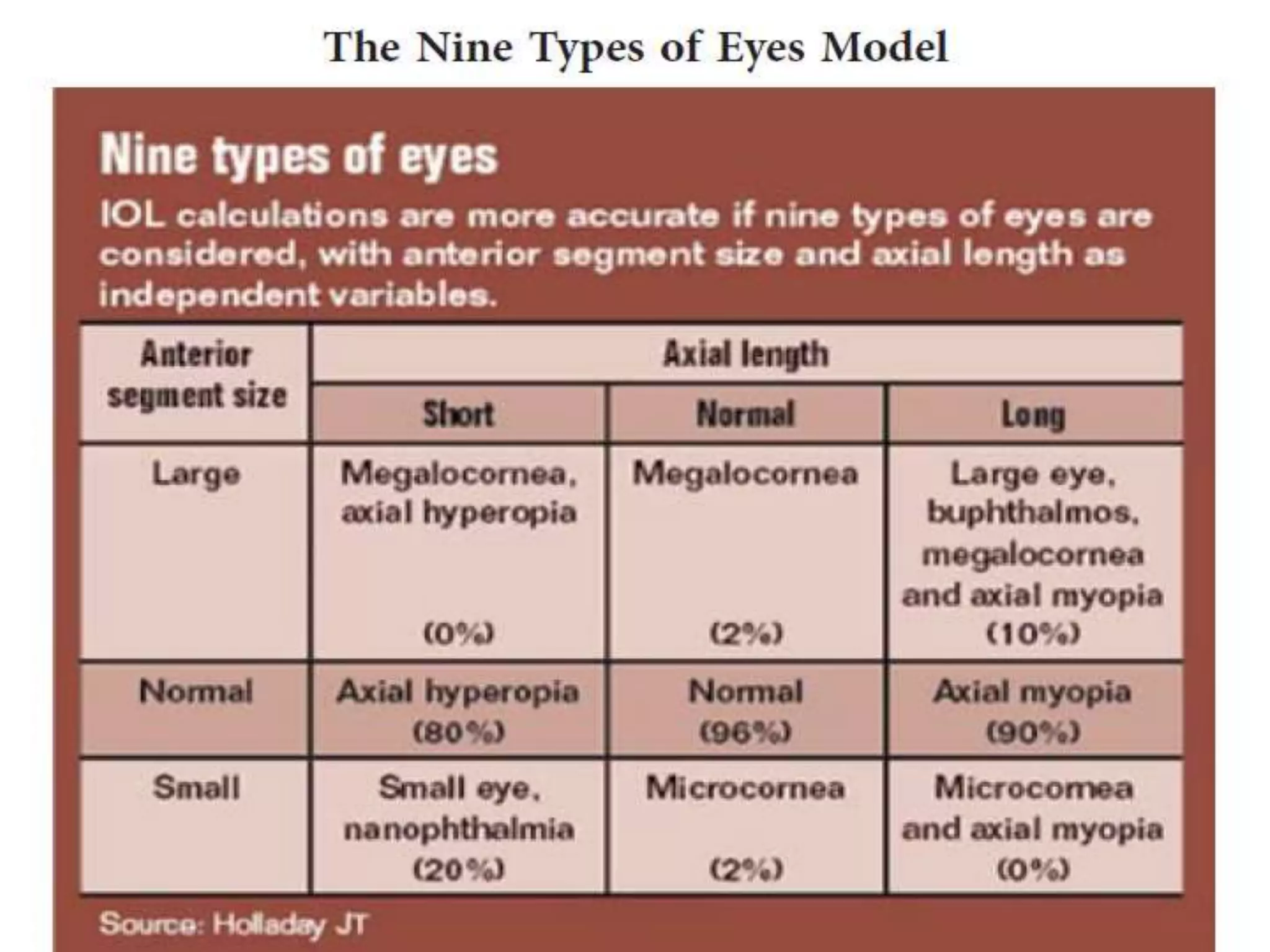
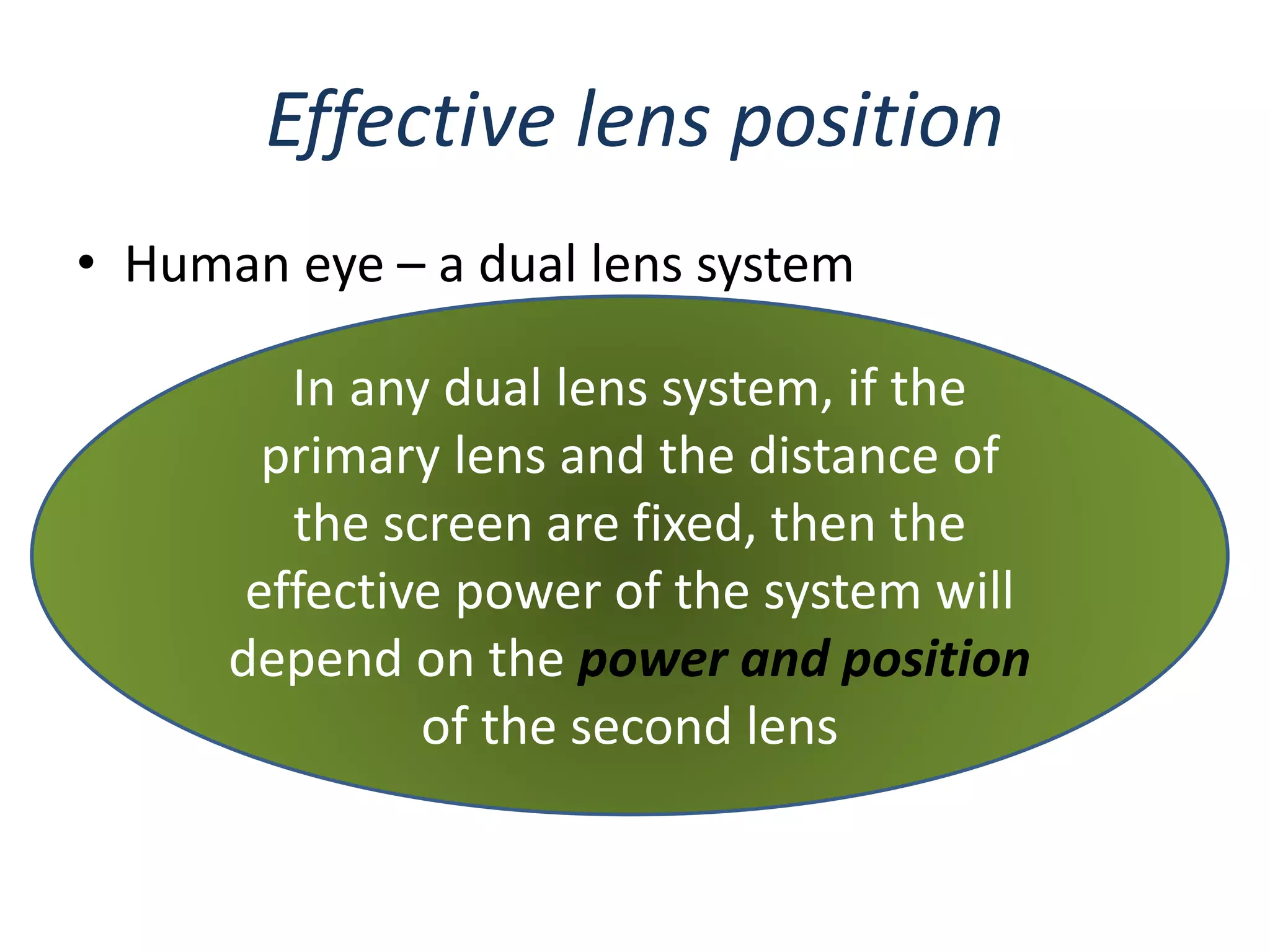
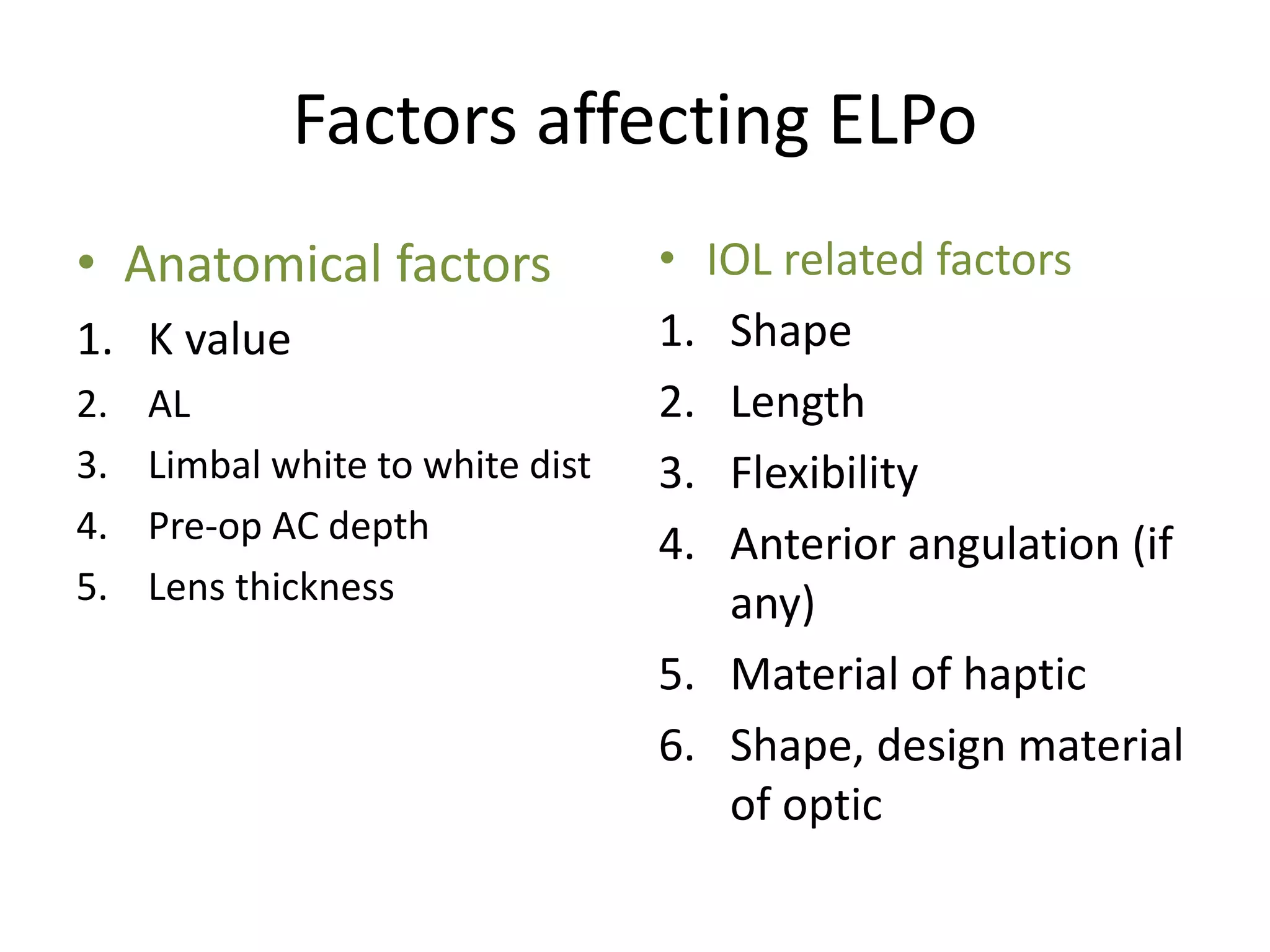
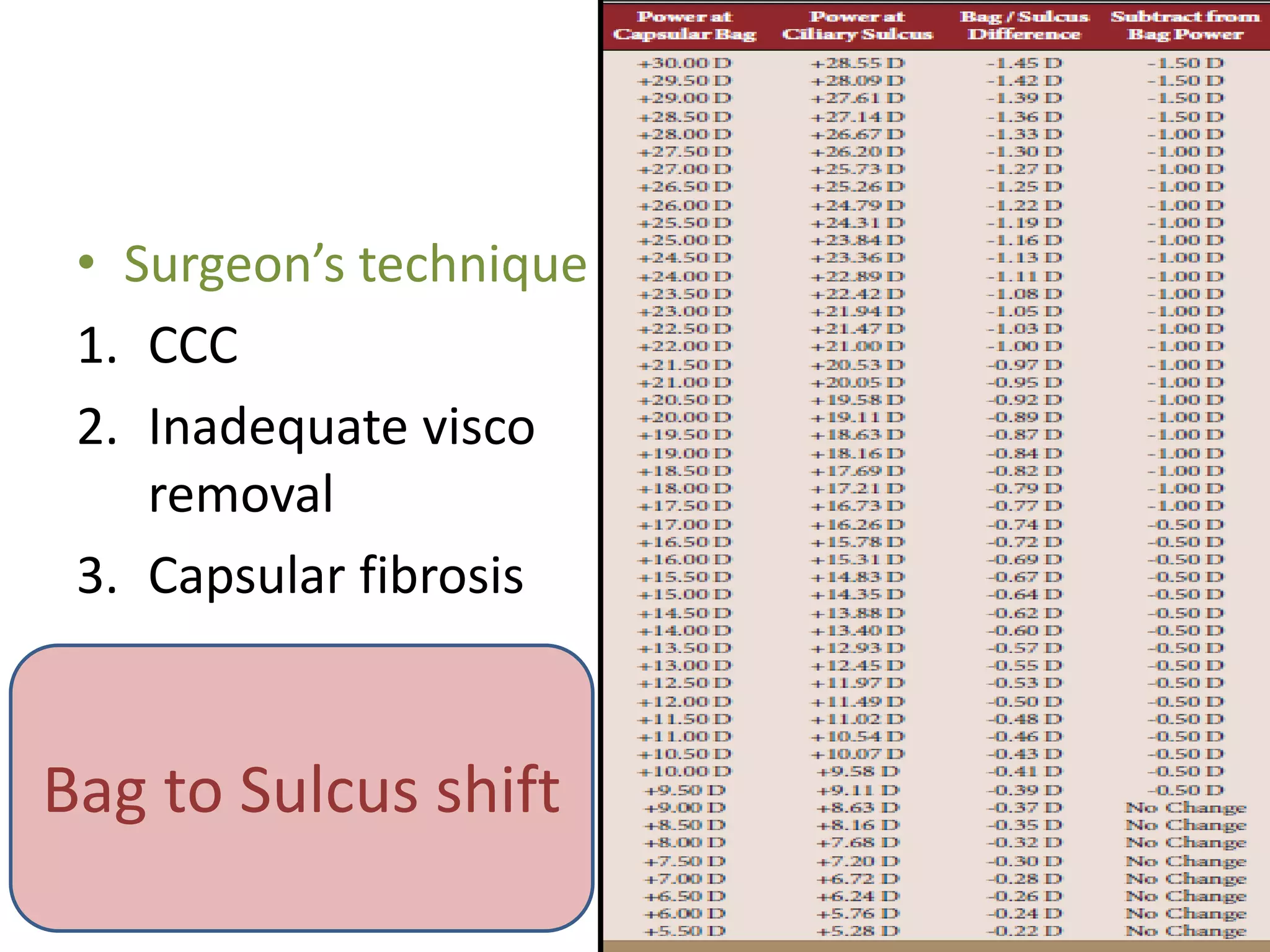
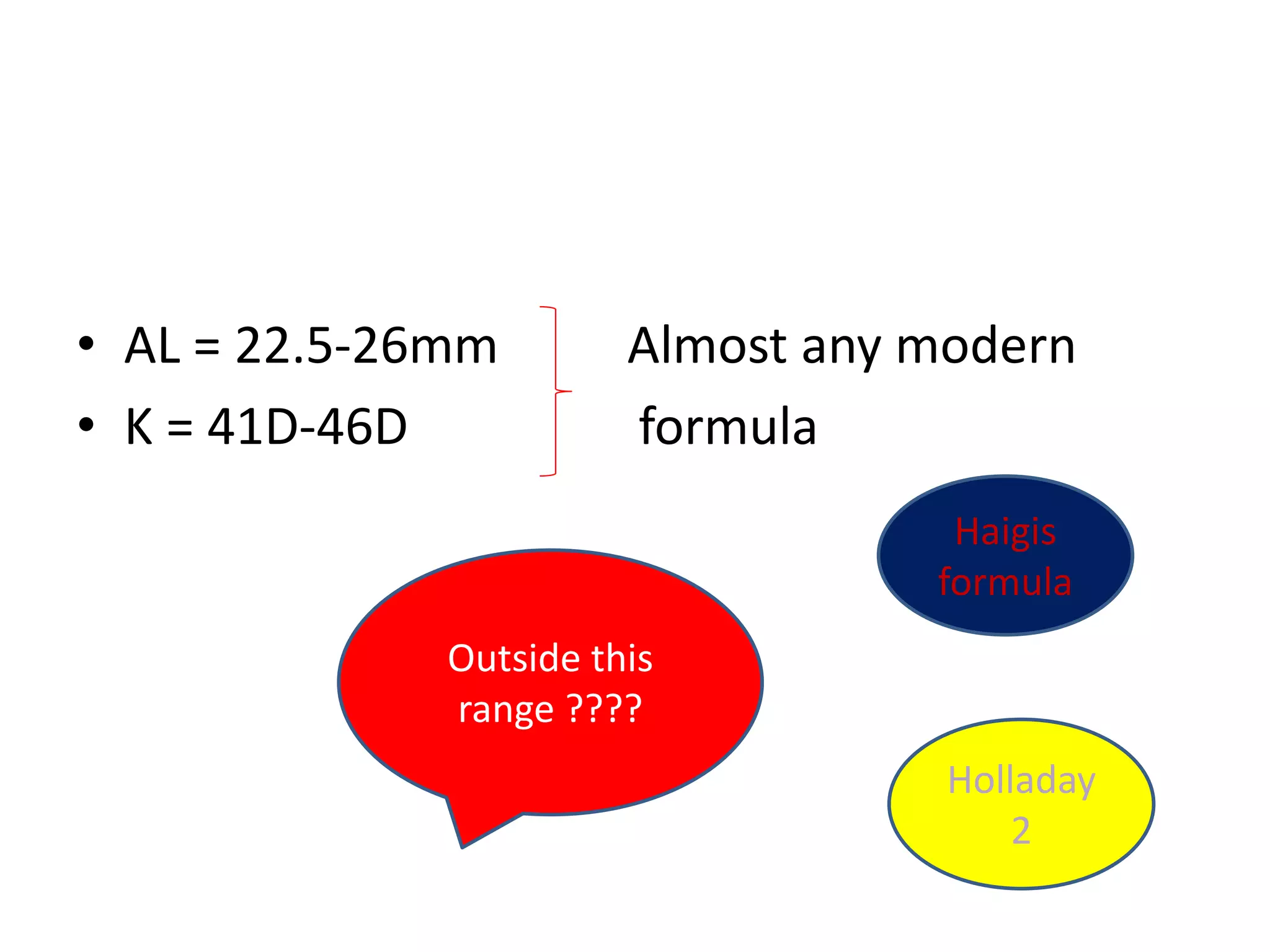
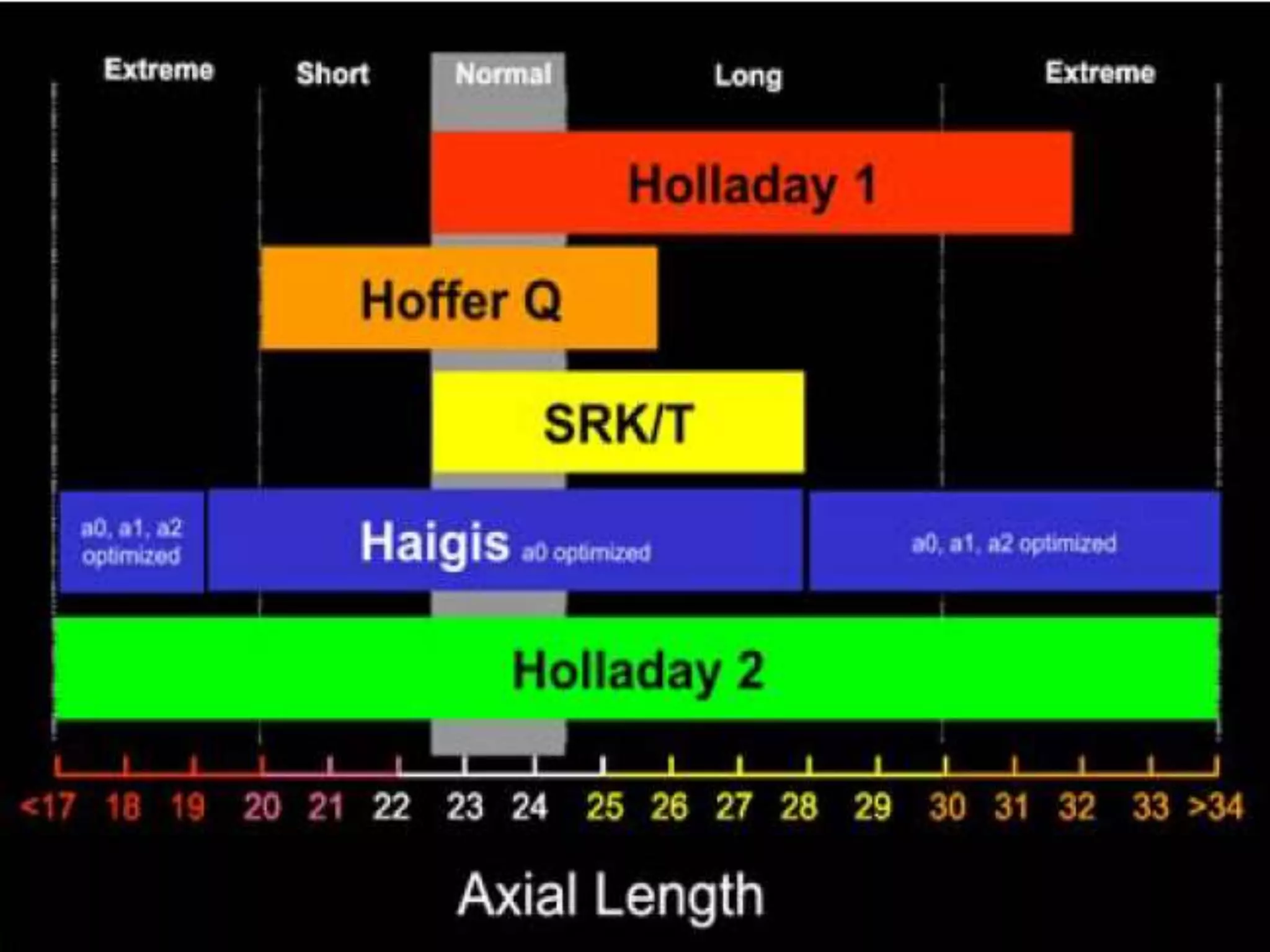
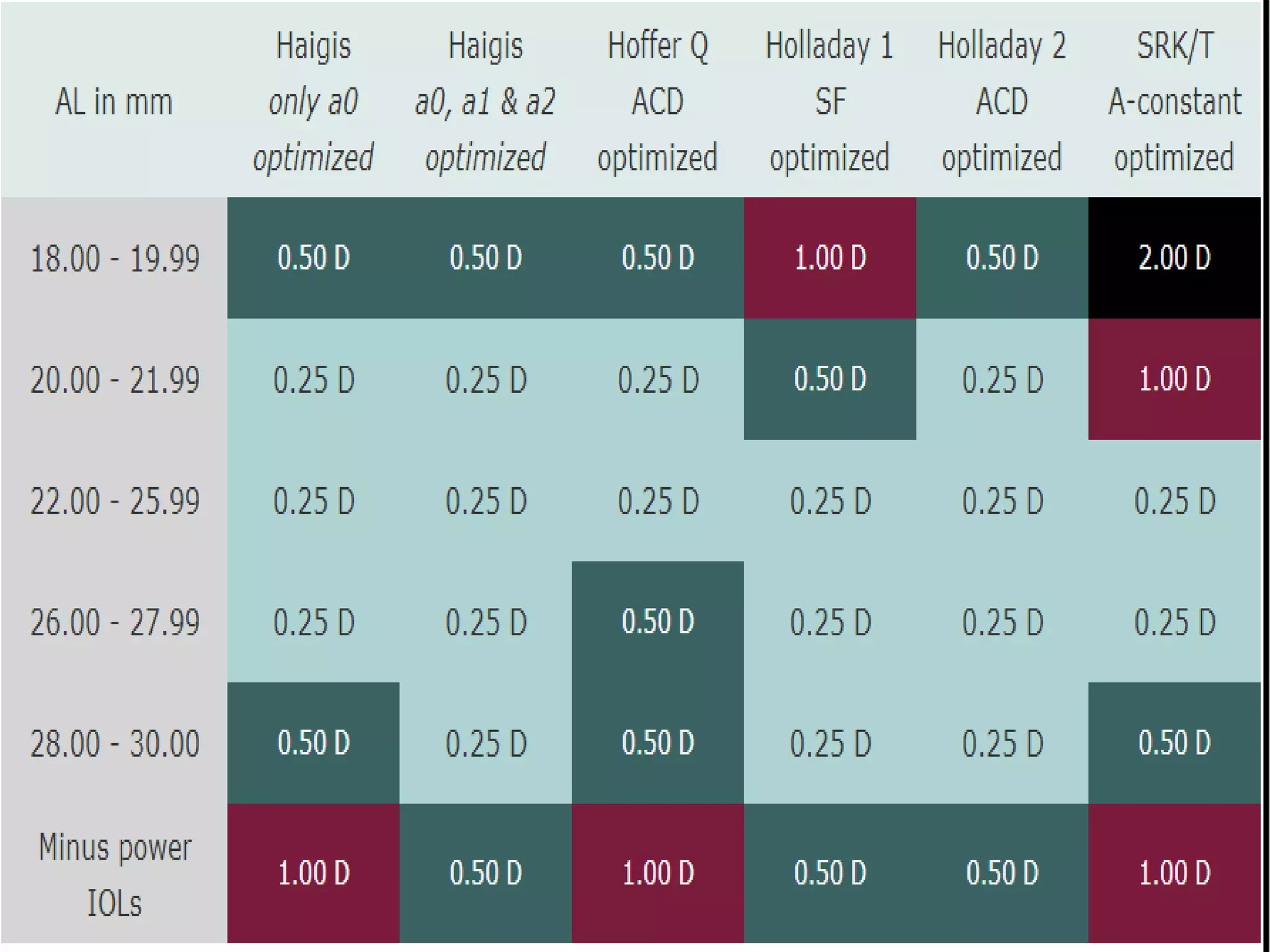
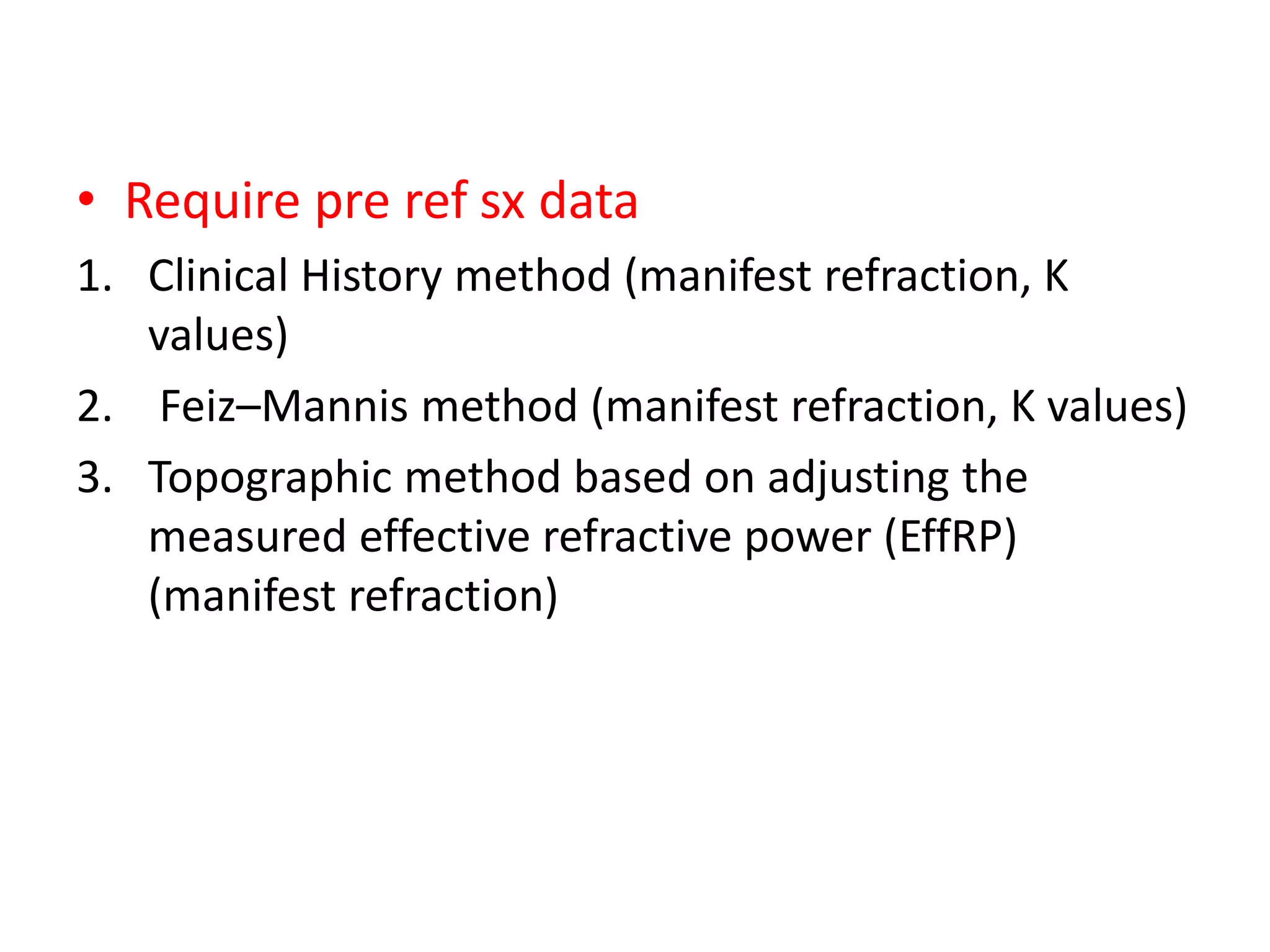
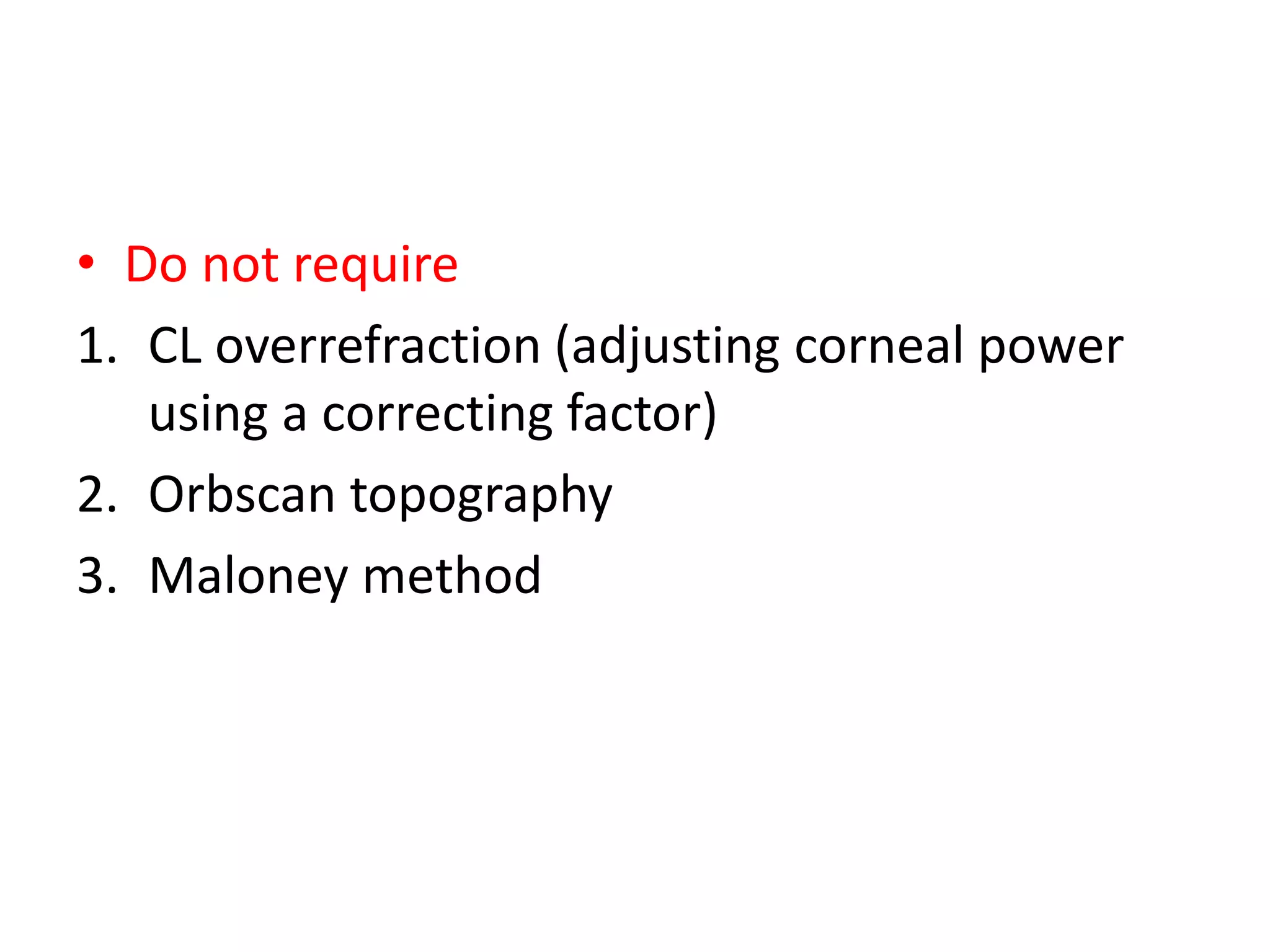
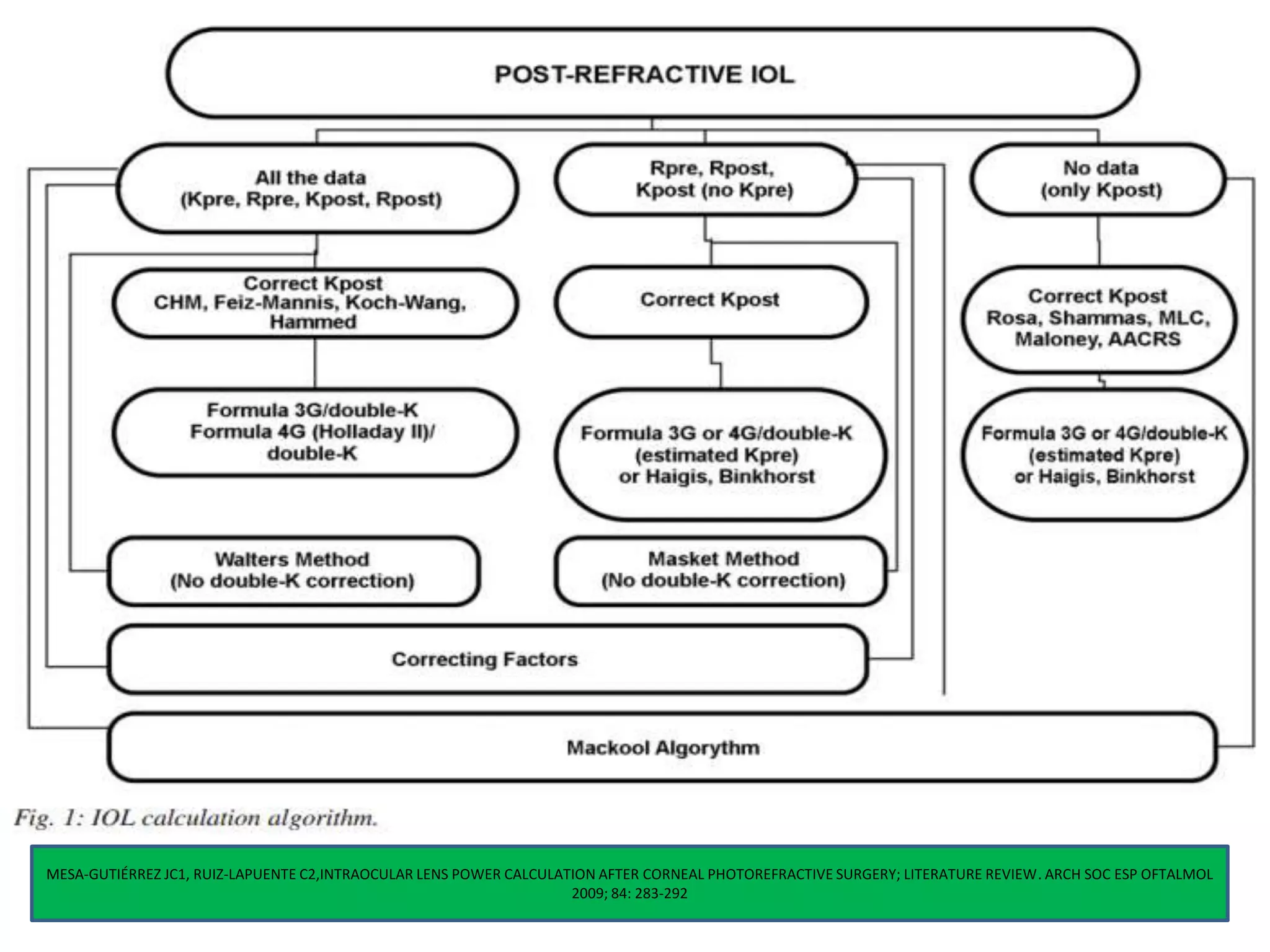
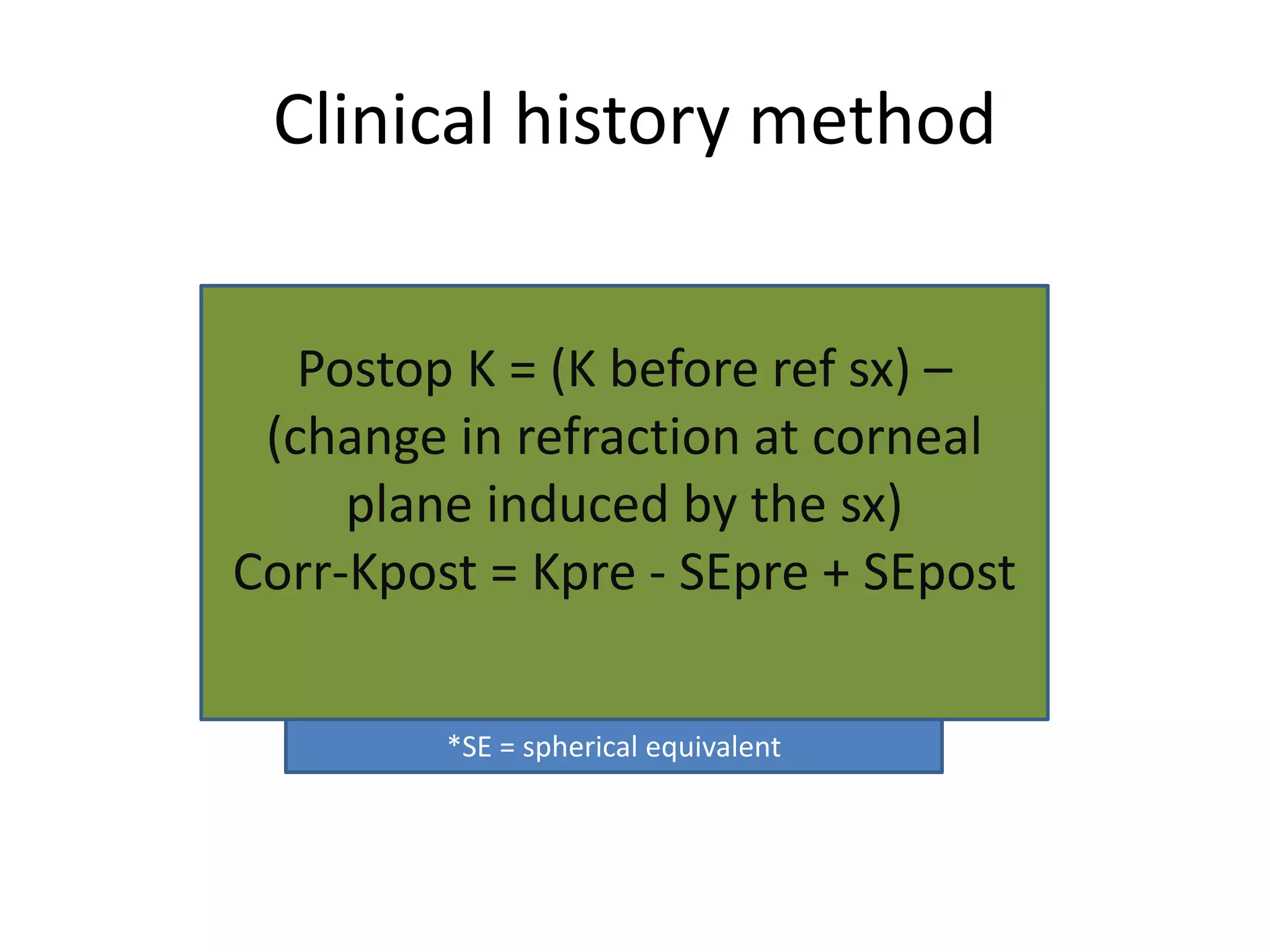
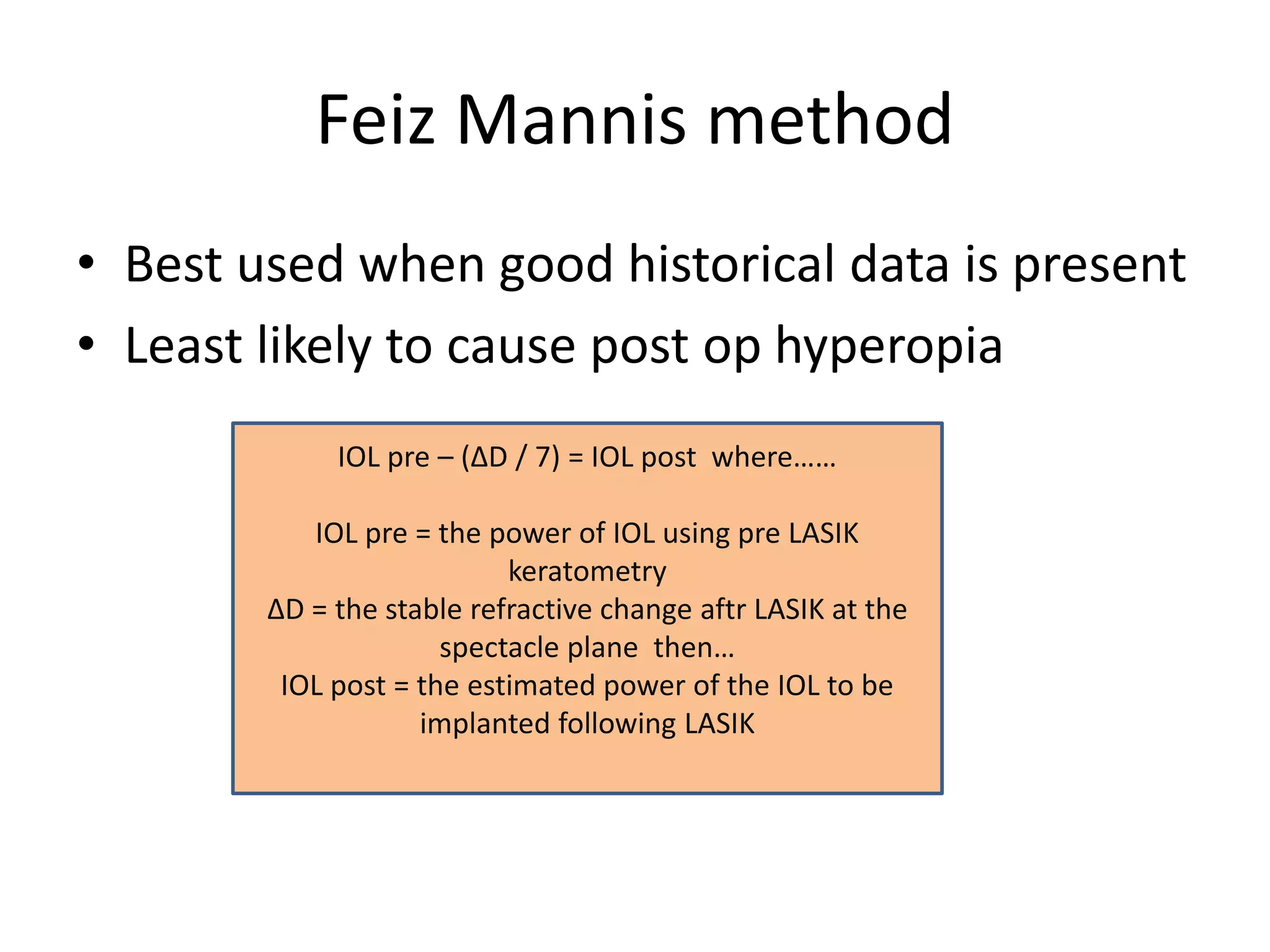
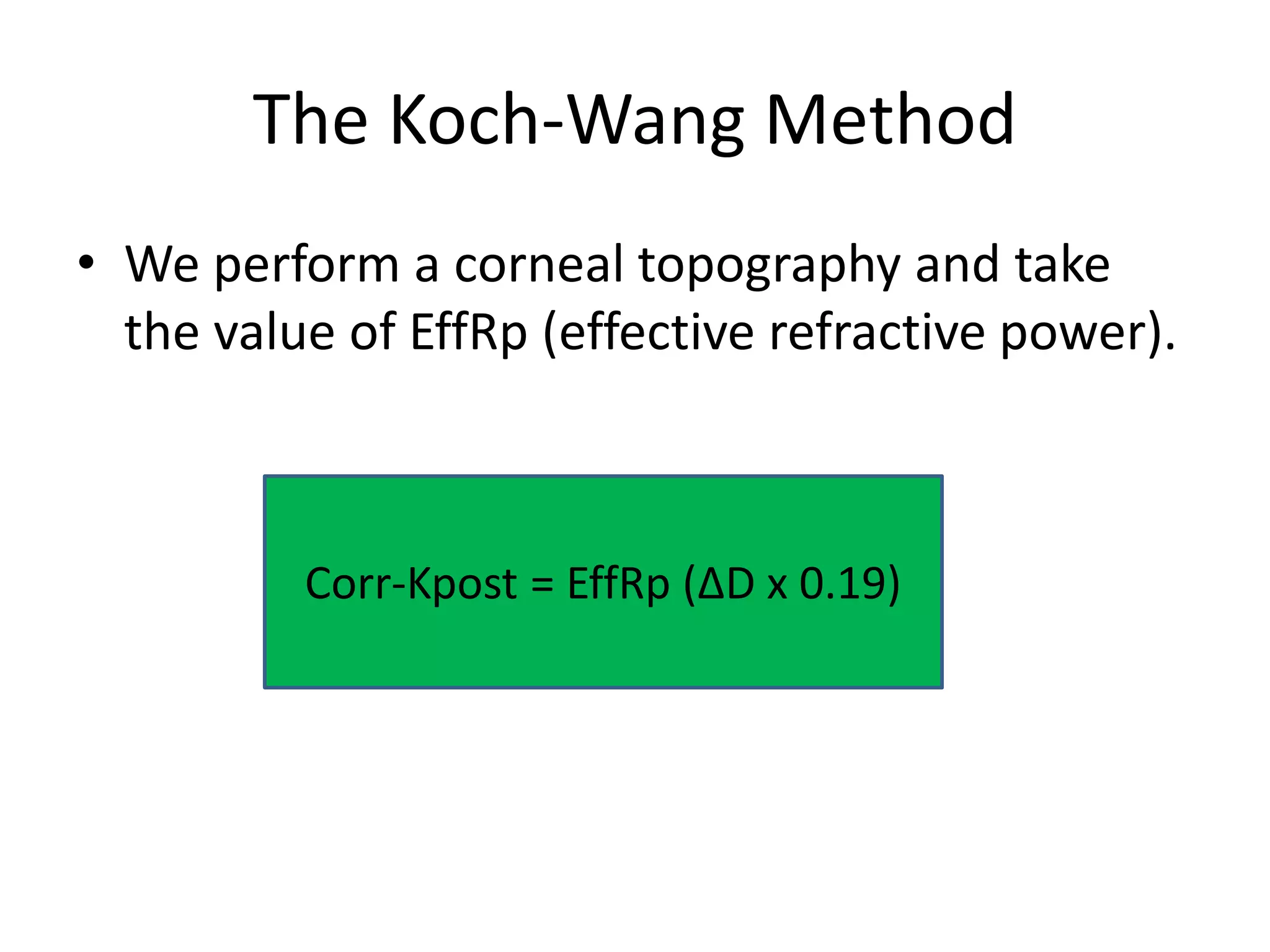
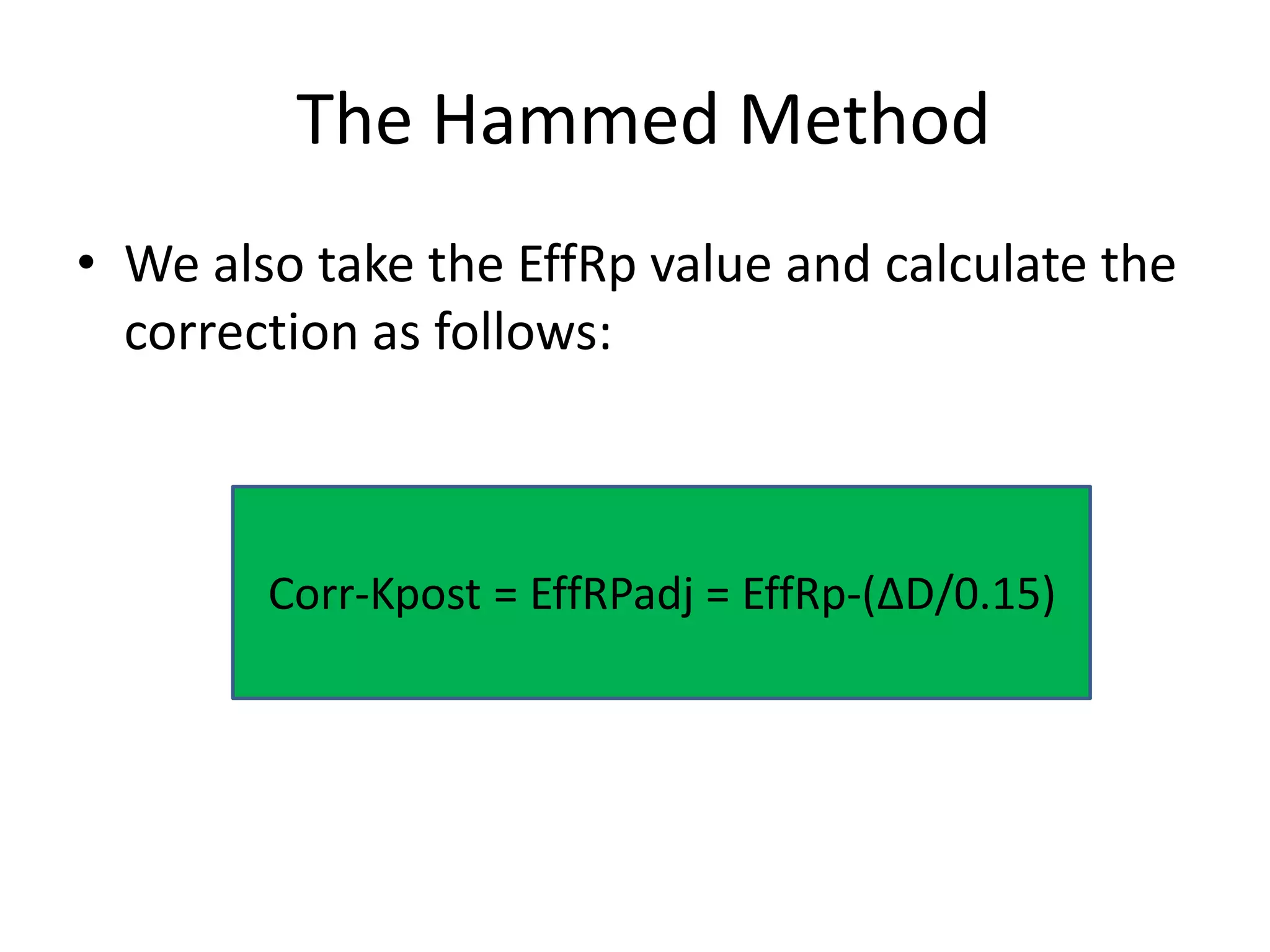
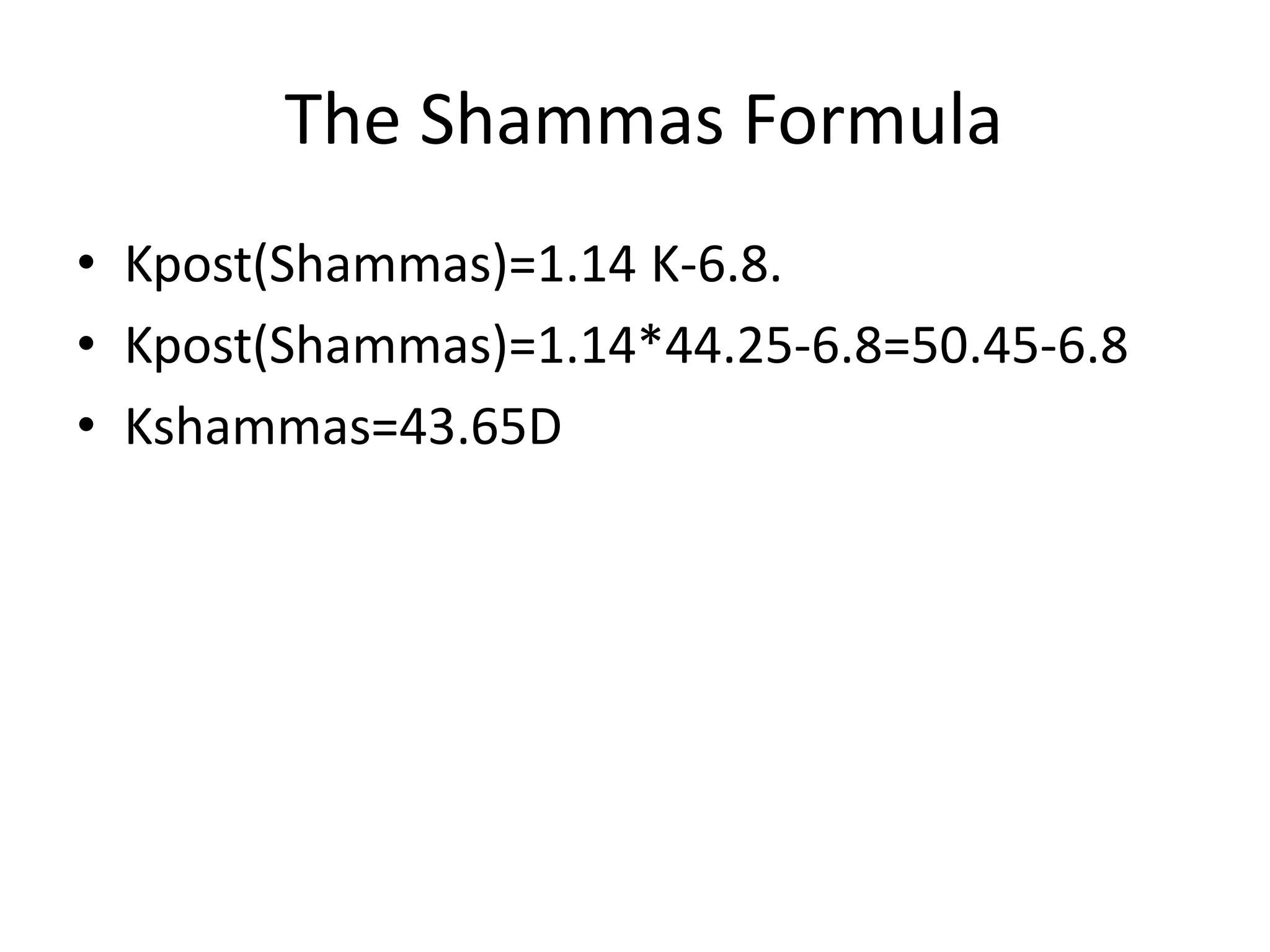
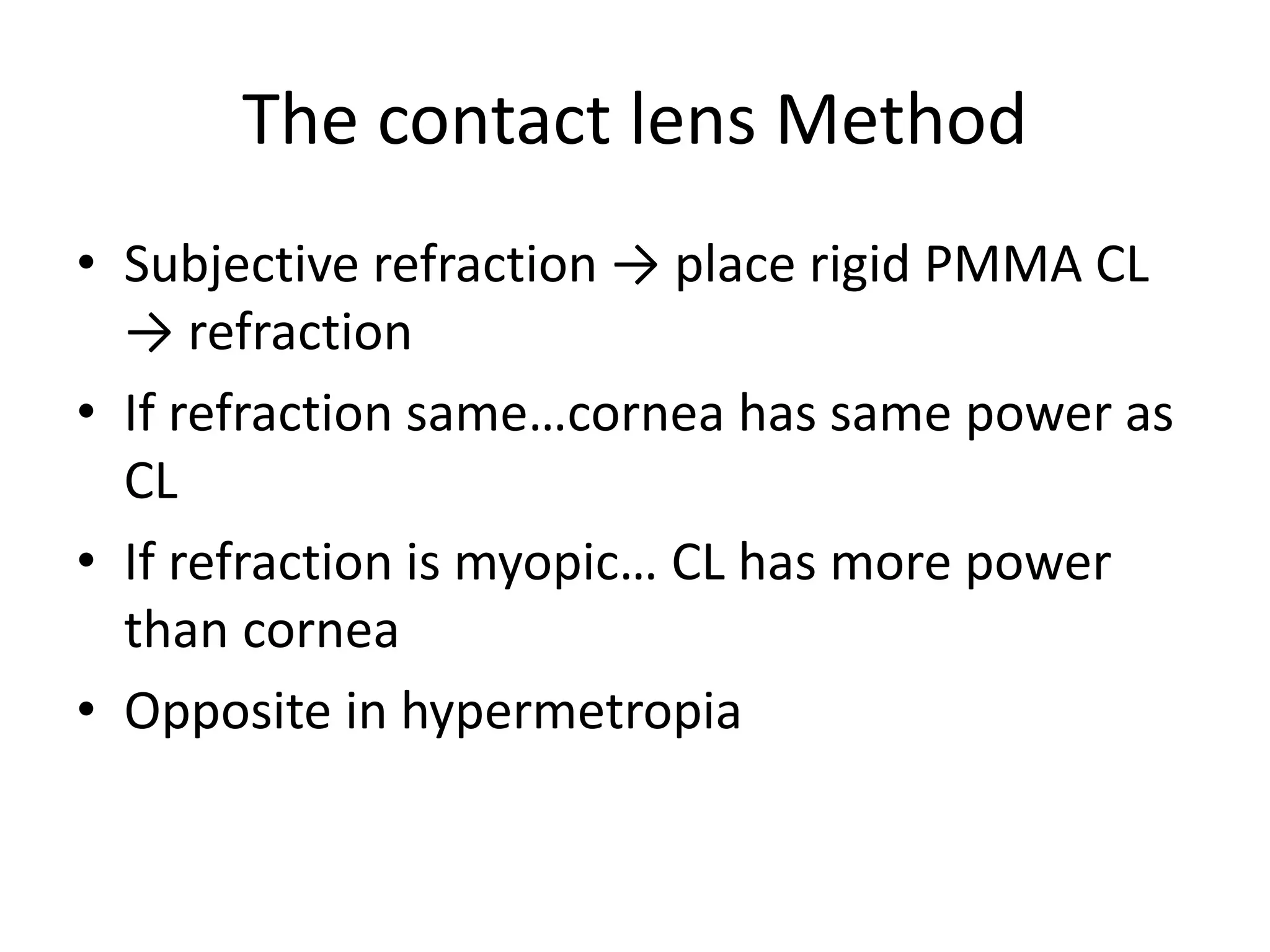
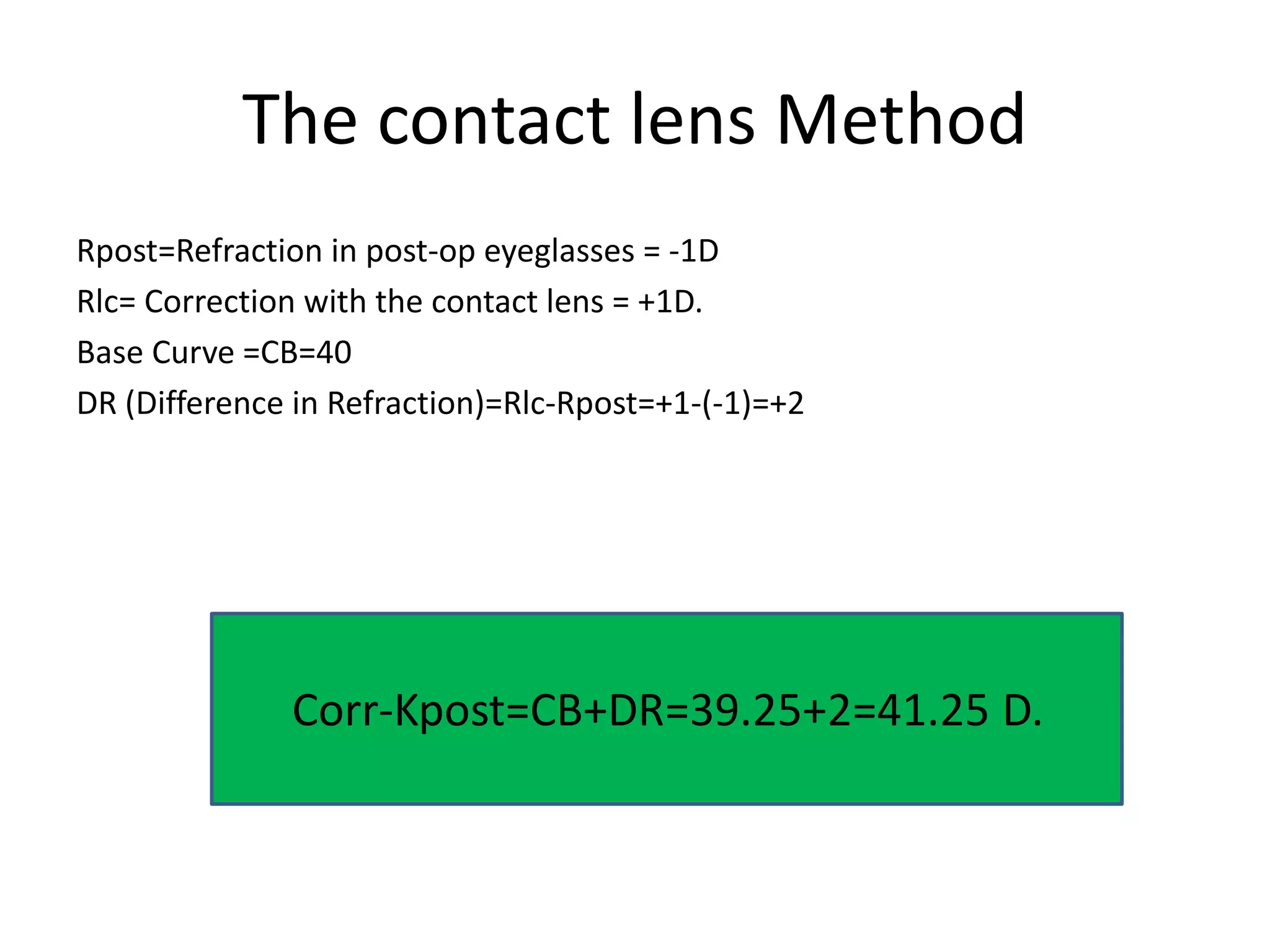
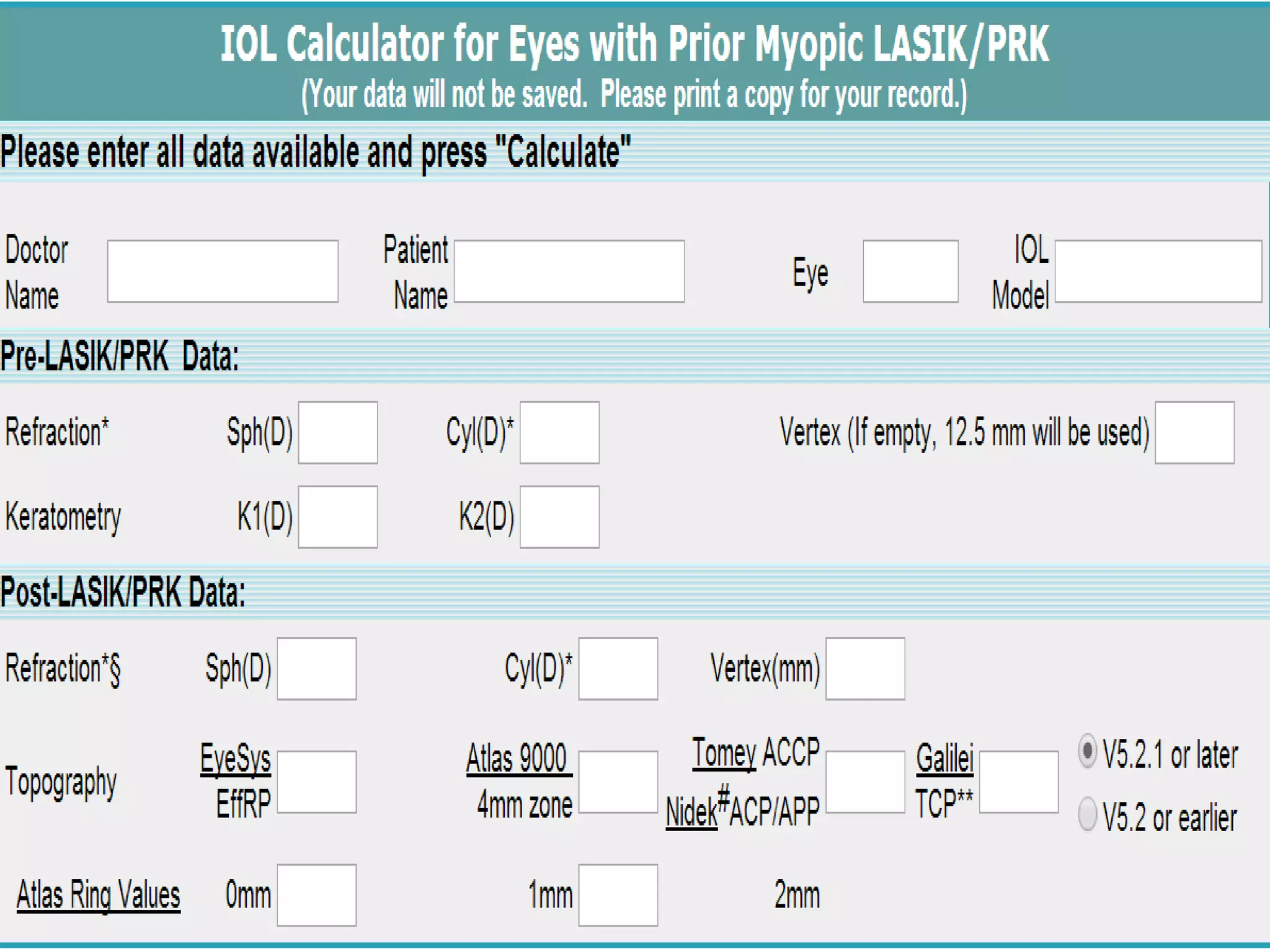
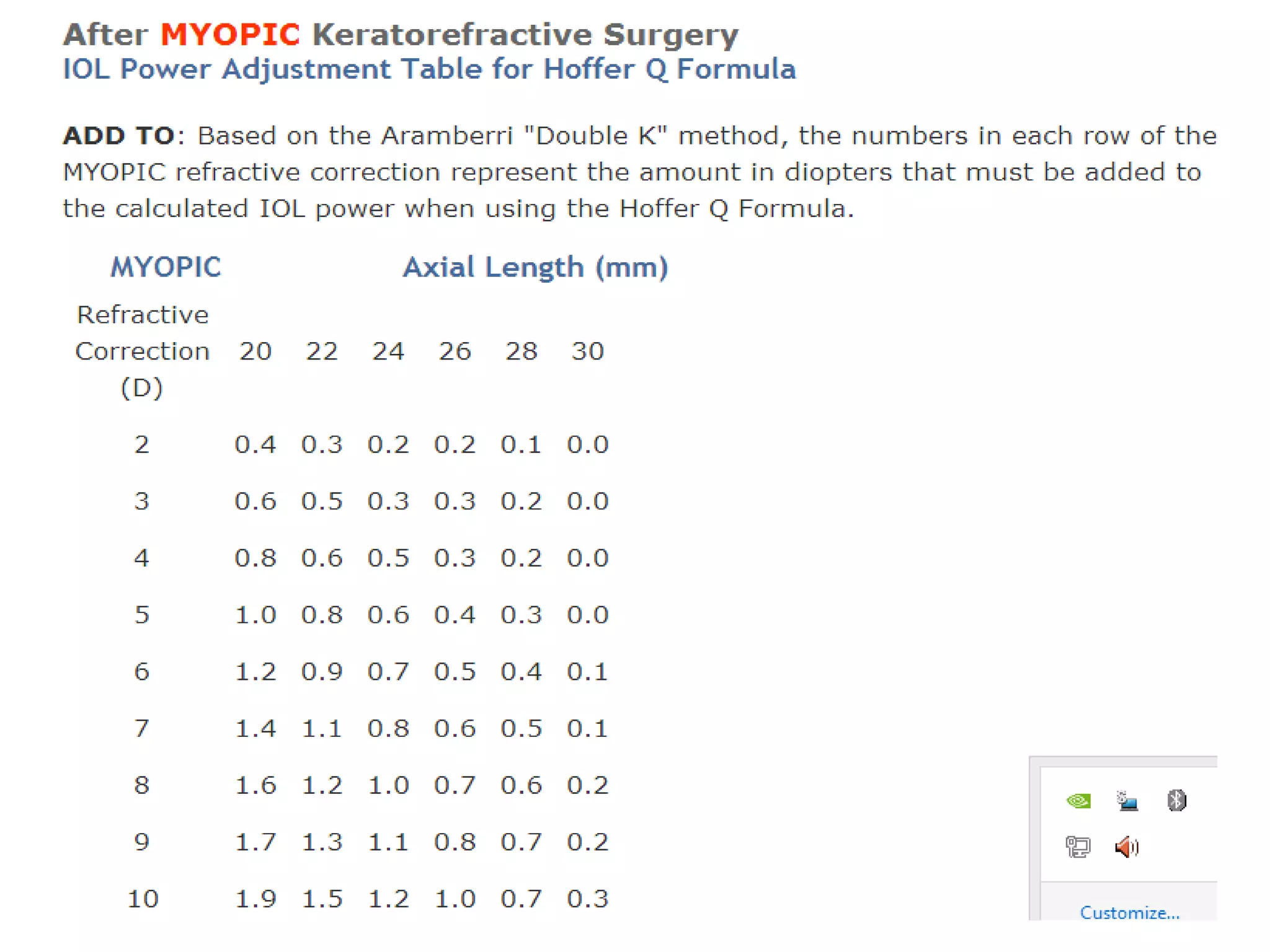
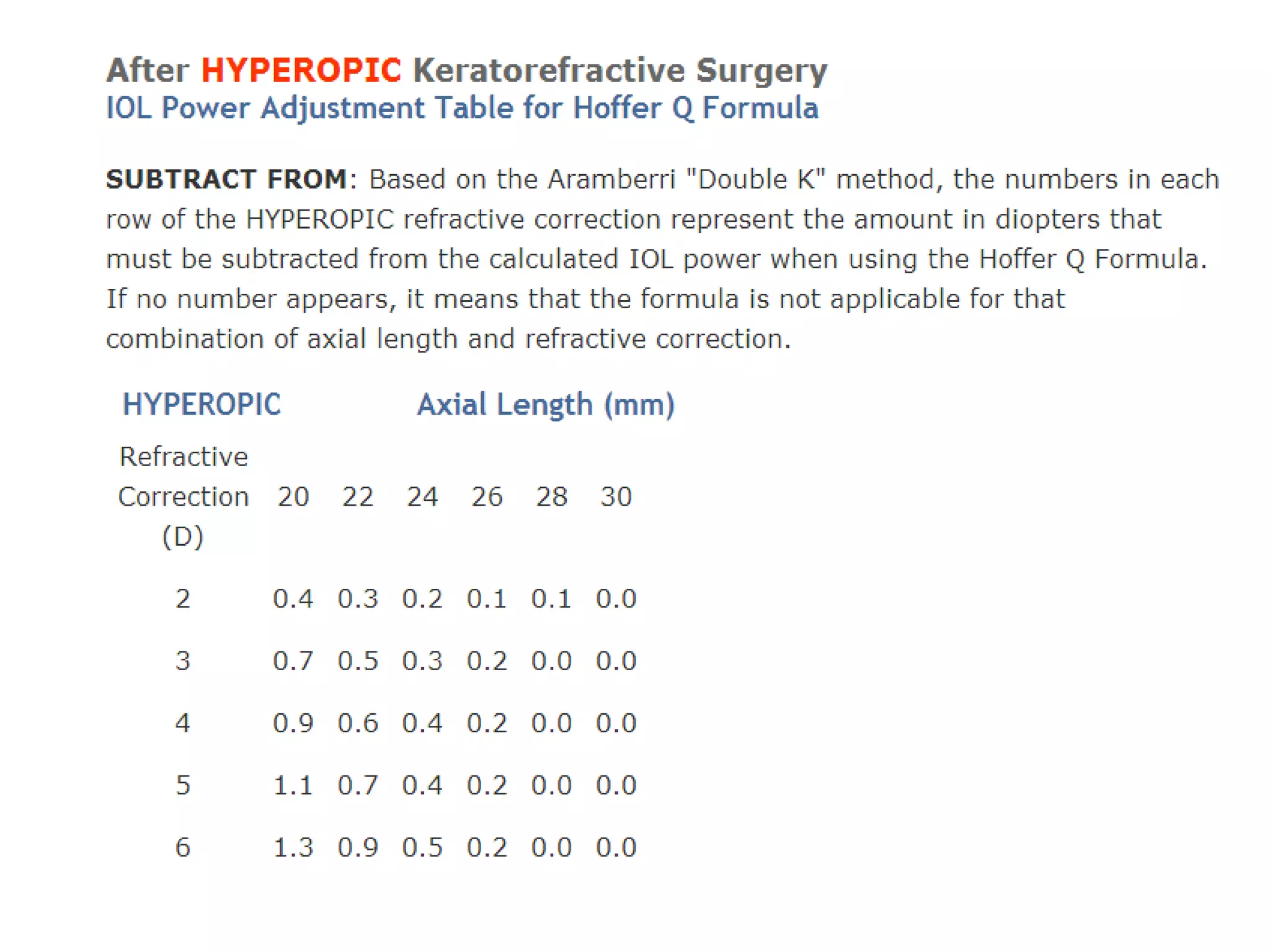
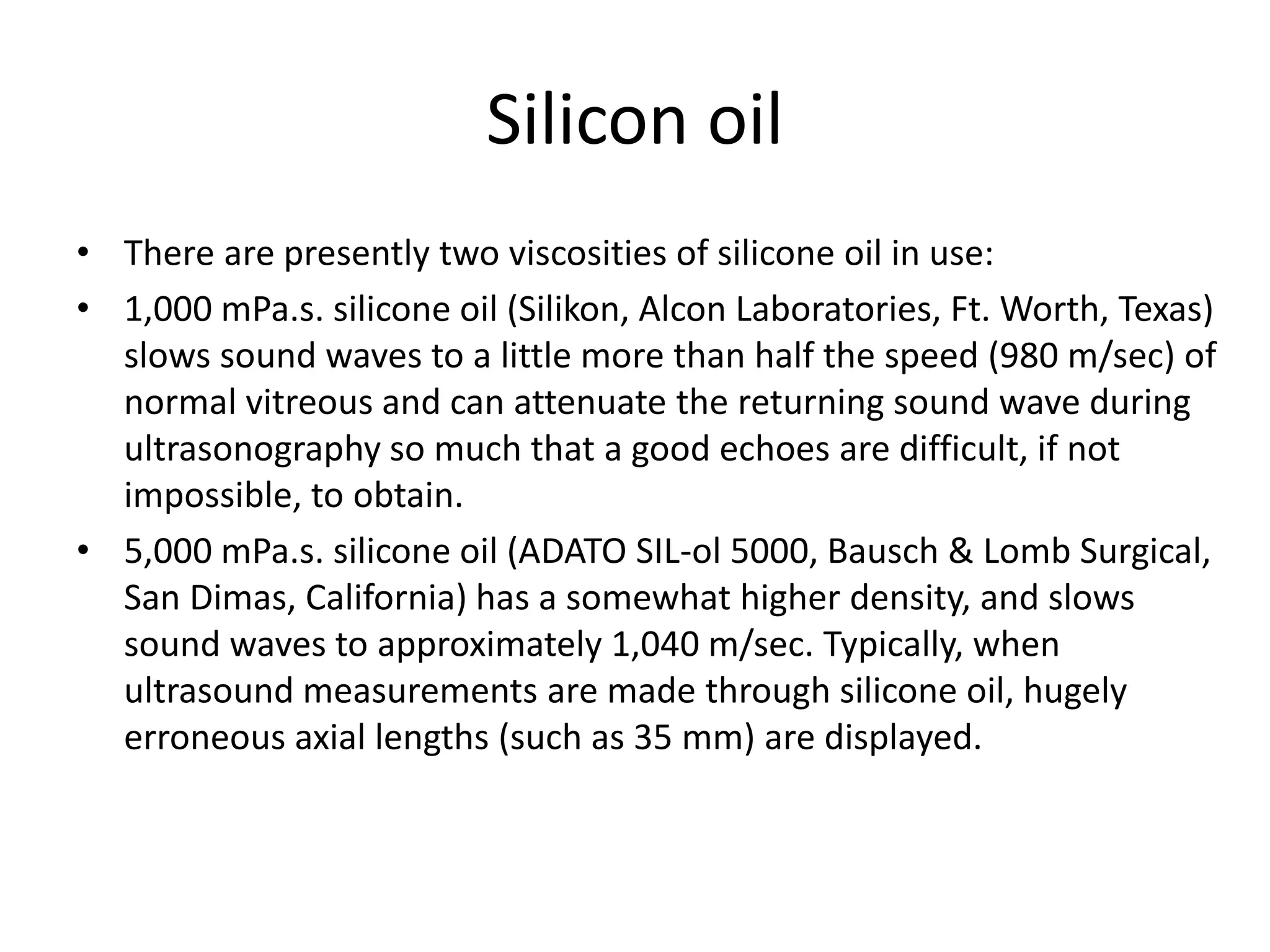
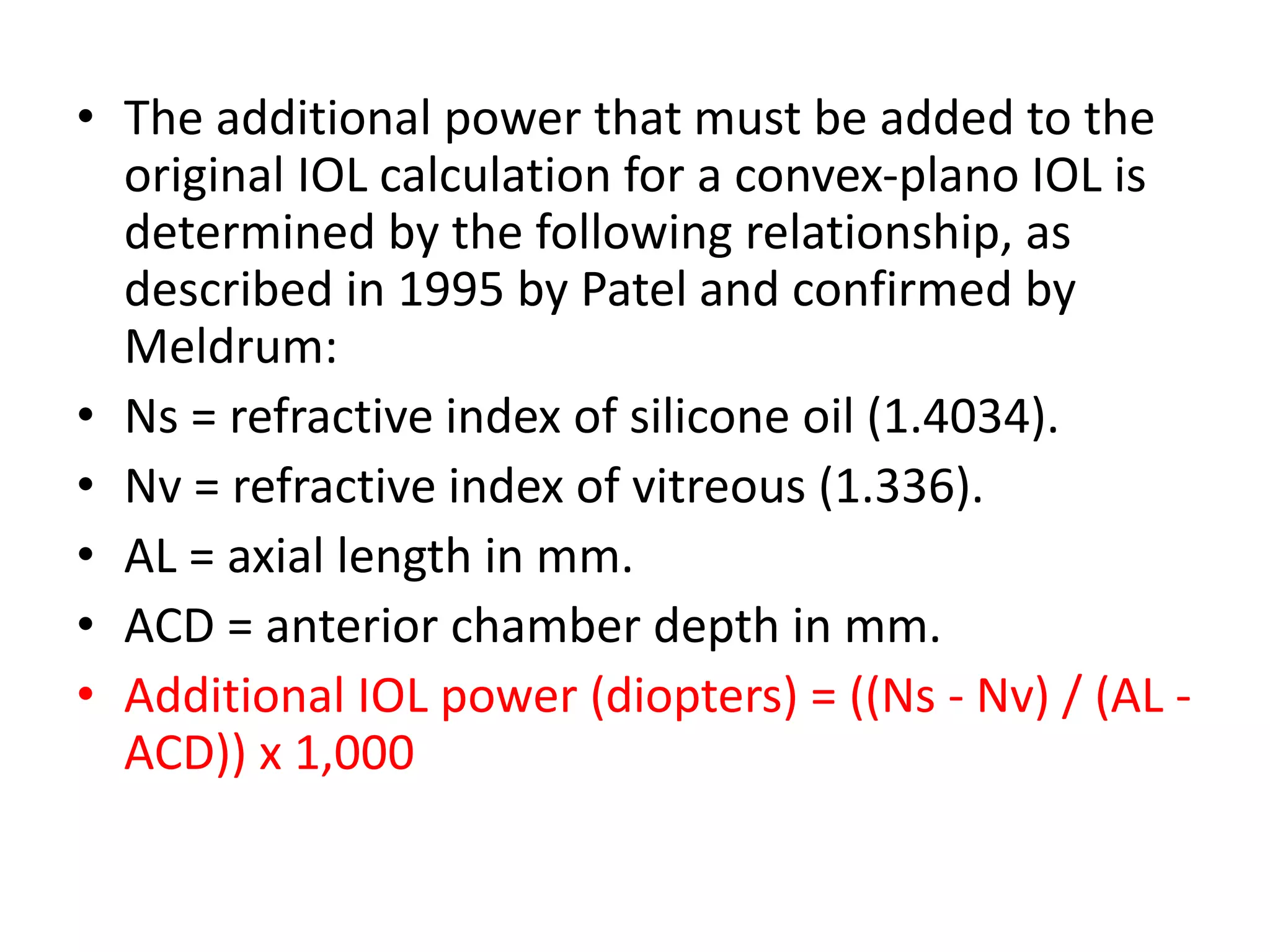
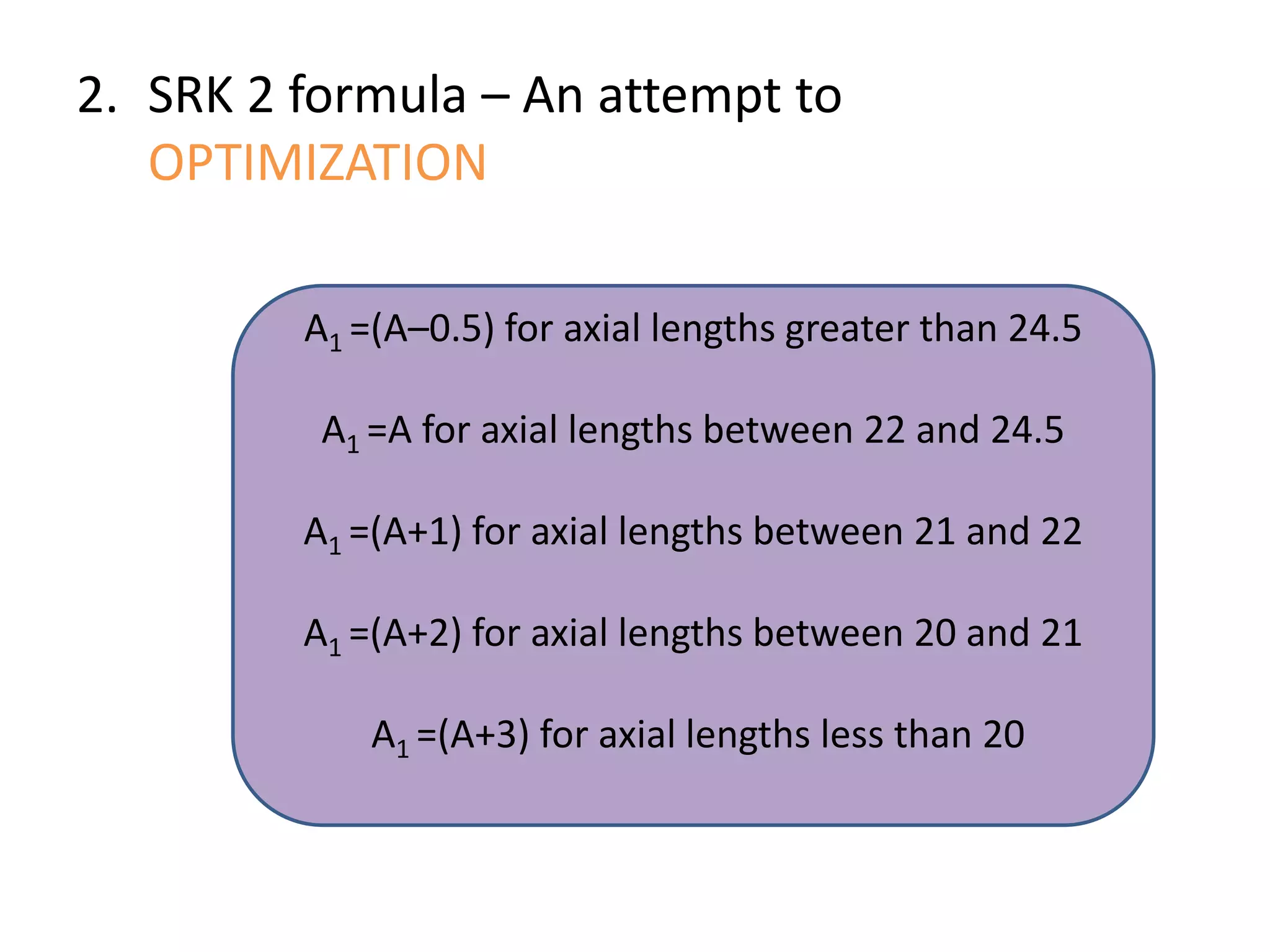
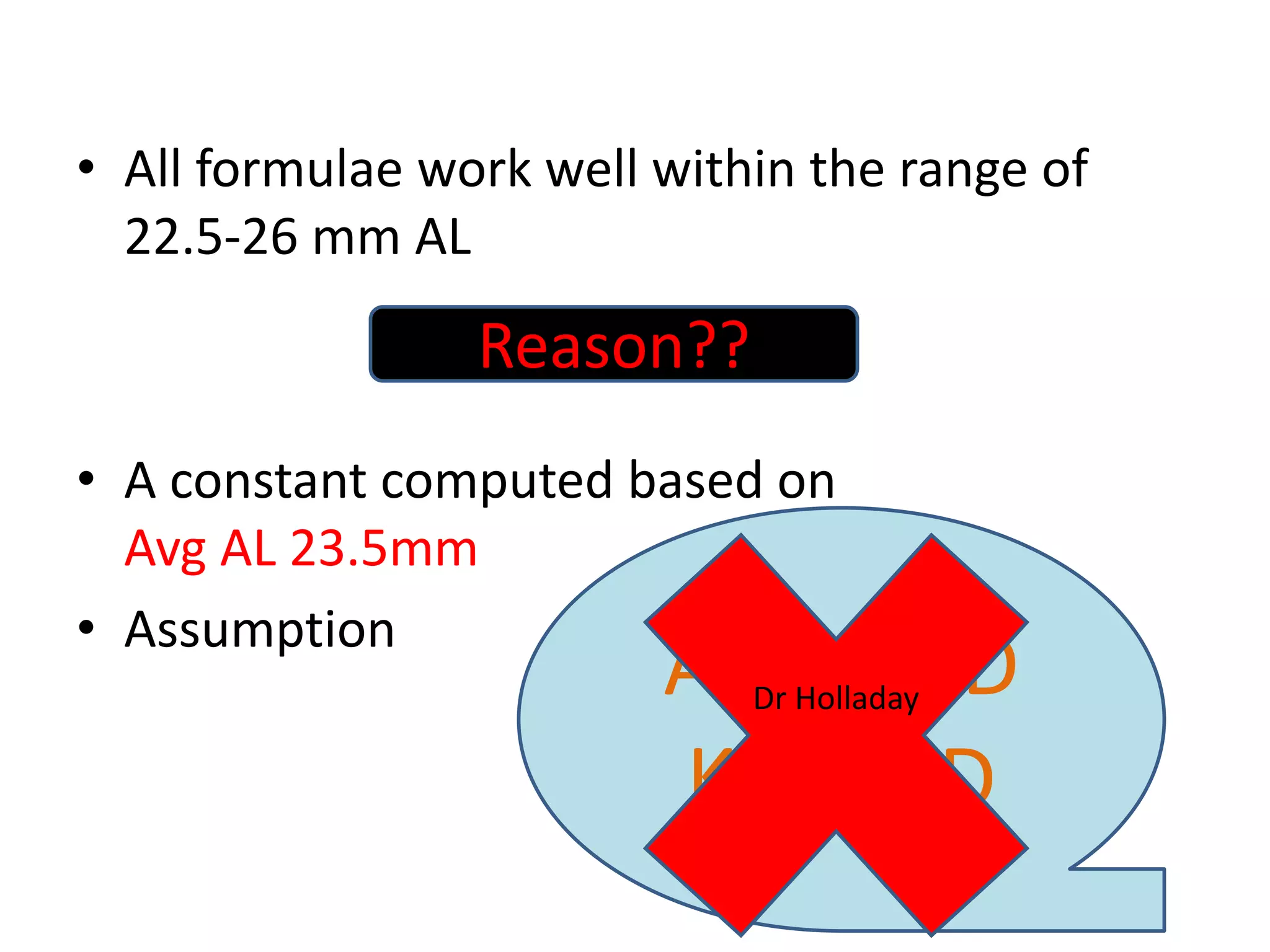
The document discusses various formulas used for calculating intraocular lens (IOL) power, including SRK, SRK2, Holladay, Haigis, and Holladay 2. It explains the factors these formulas account for such as axial length, corneal power, anterior chamber depth, and how they have evolved over generations to improve accuracy. Special considerations for calculating IOL power in cases involving prior refractive surgery, silicone oil filling, posterior staphyloma, and using optical biometry devices are also summarized.
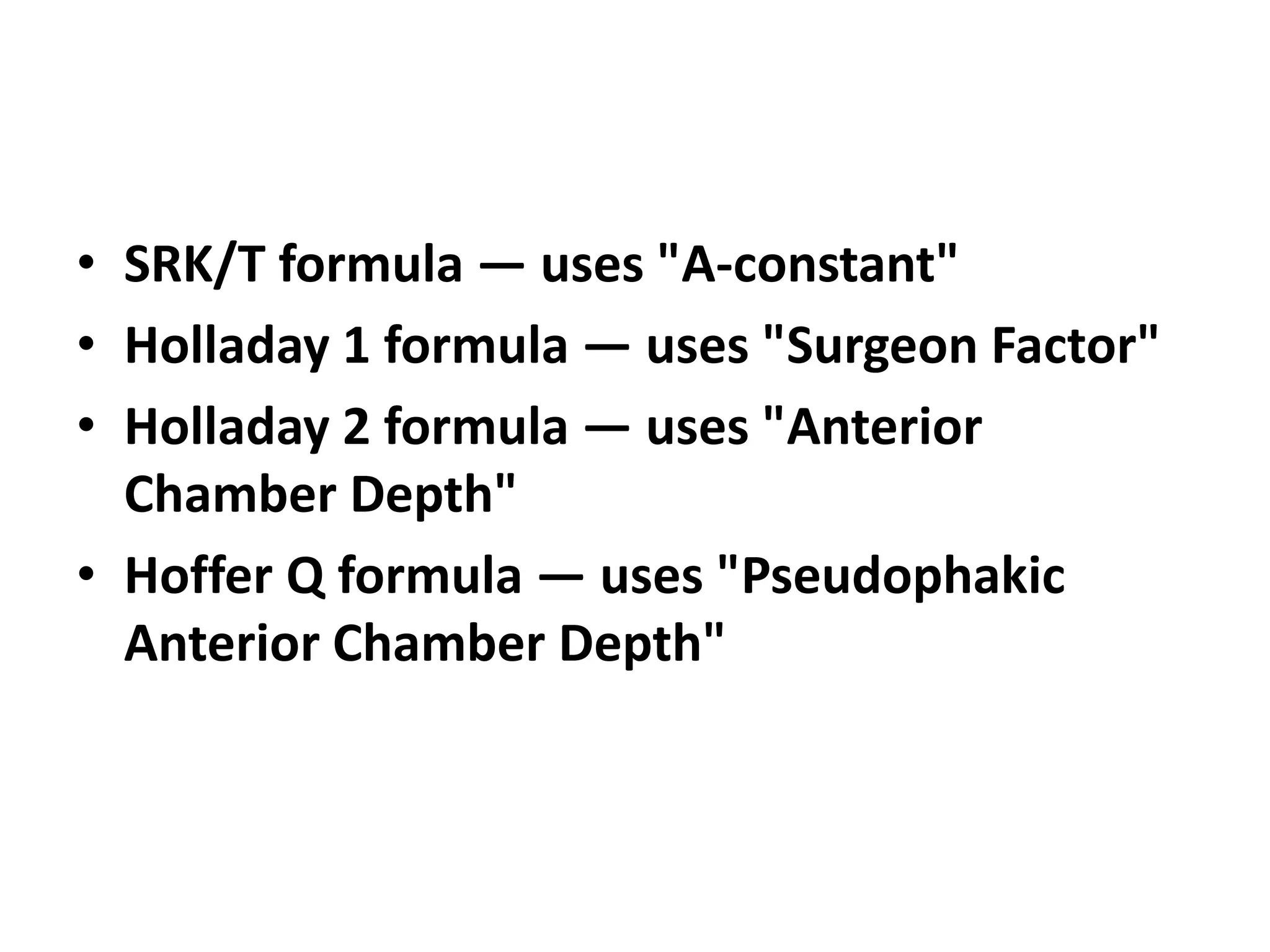
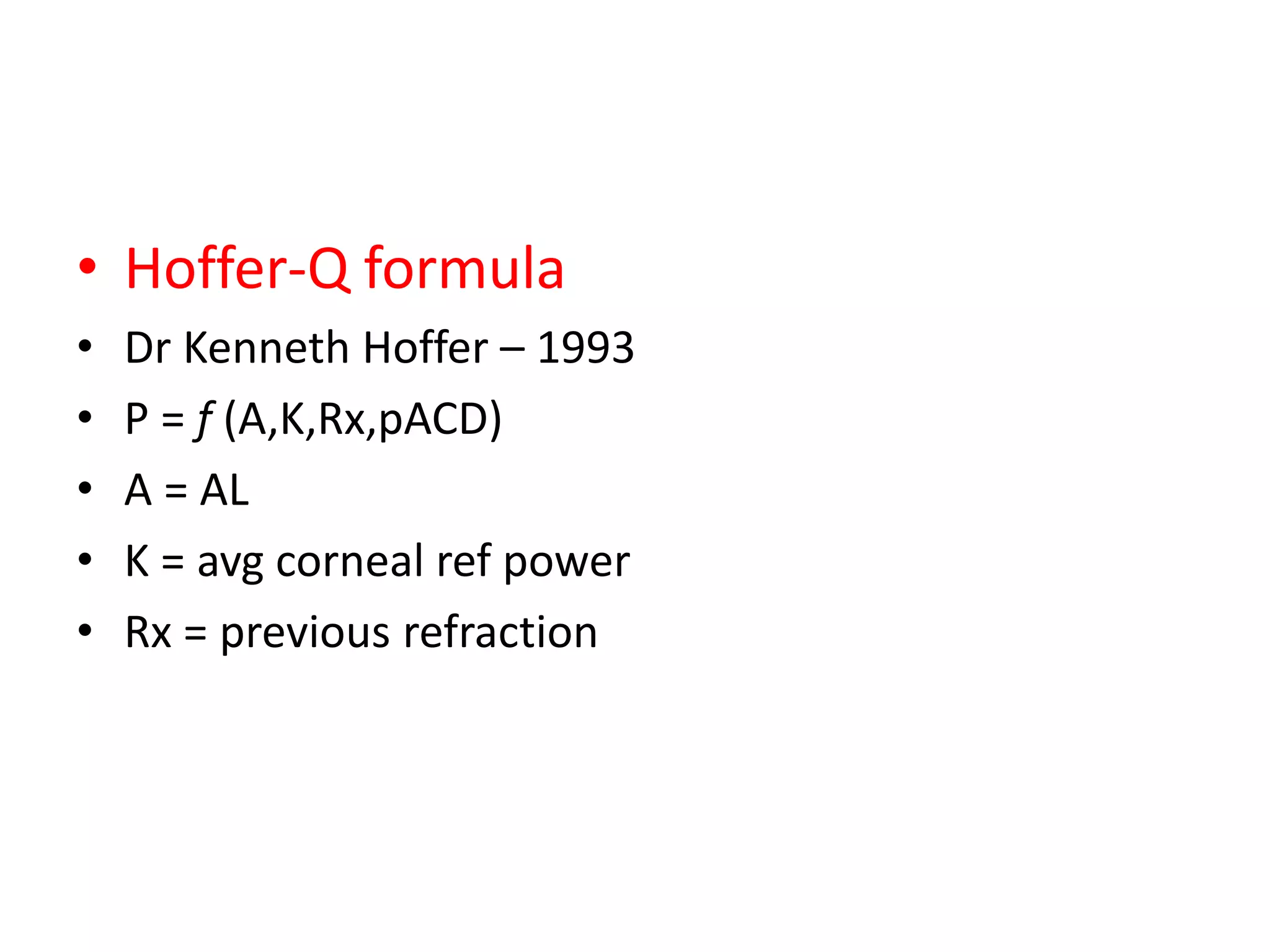
![• pACD = The personalized ACD (pACD) is set
equal to the manufacturer's ACD-constant, if
the calculation was selected to be based on
the ACD-constant. In case the A-constant was
chosen, pACD is derived from the A-constant
[HOFFER, 1998] according to [HOLLADAY et al,
1988]
pACD = ACD-const = 0.58357 * A-const -
63.896 .](https://image.slidesharecdn.com/iolcalculation-140310083334-phpapp02/75/IOL-power-calculation-formulae-10-2048.jpg)