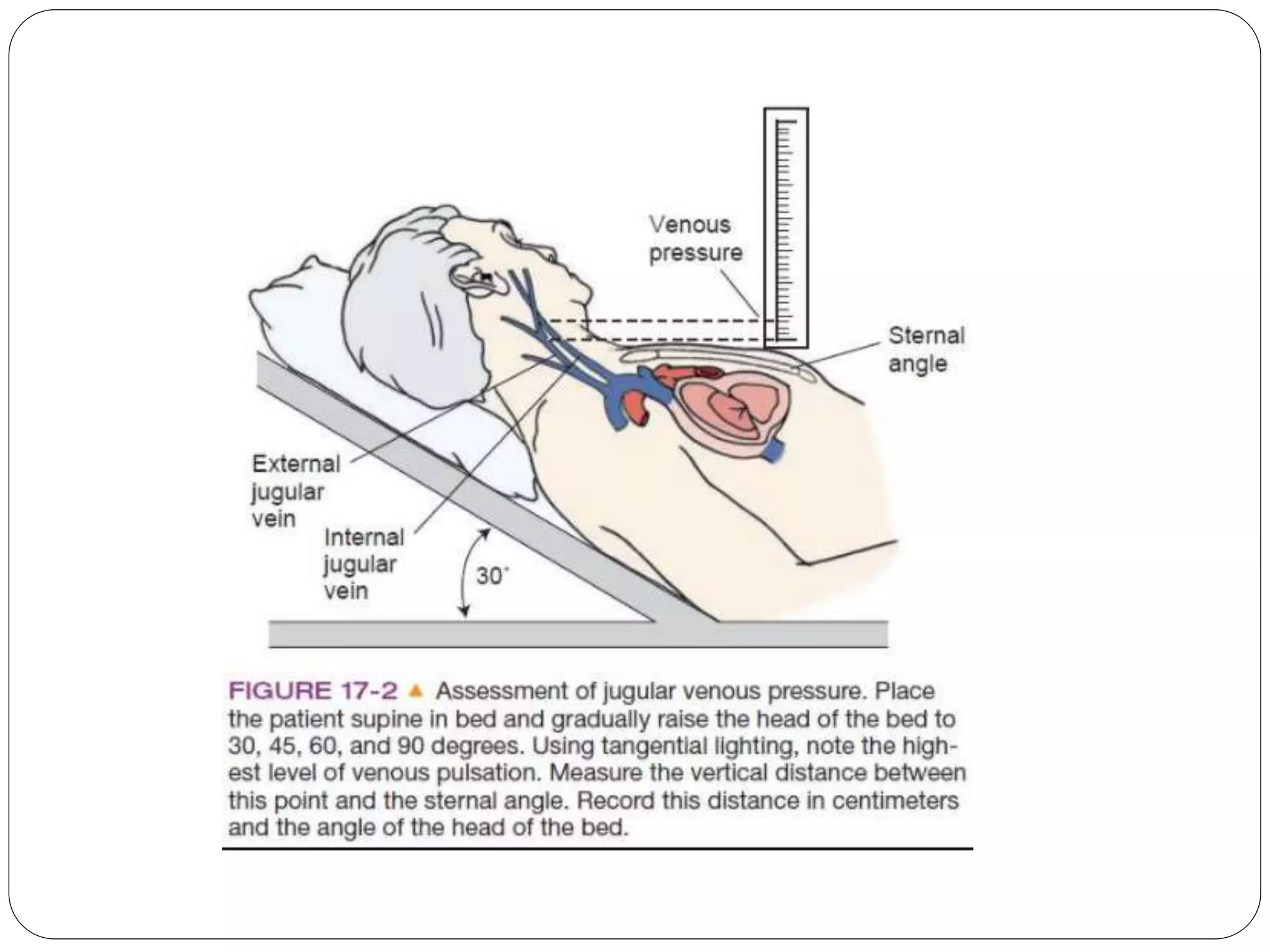
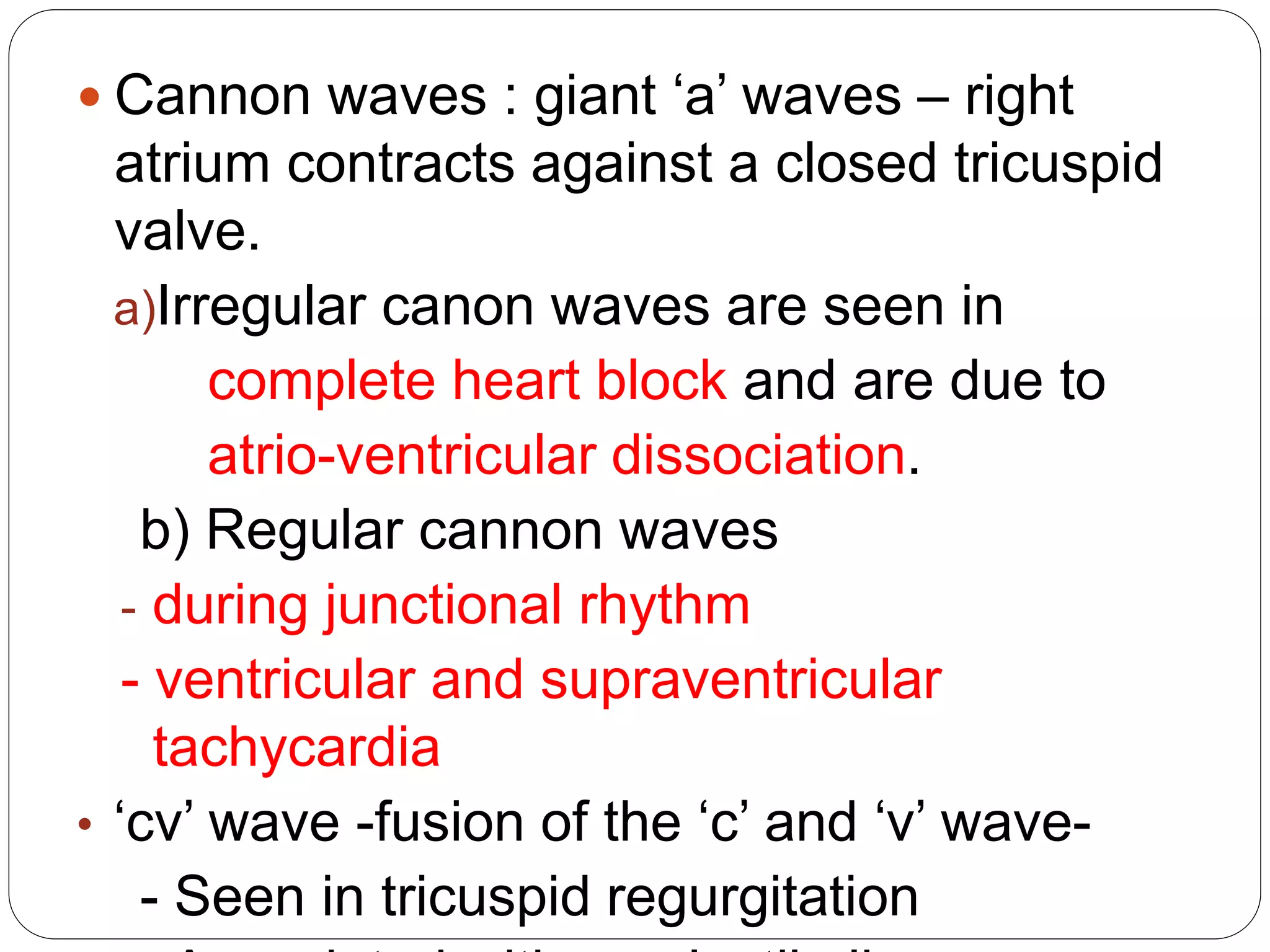
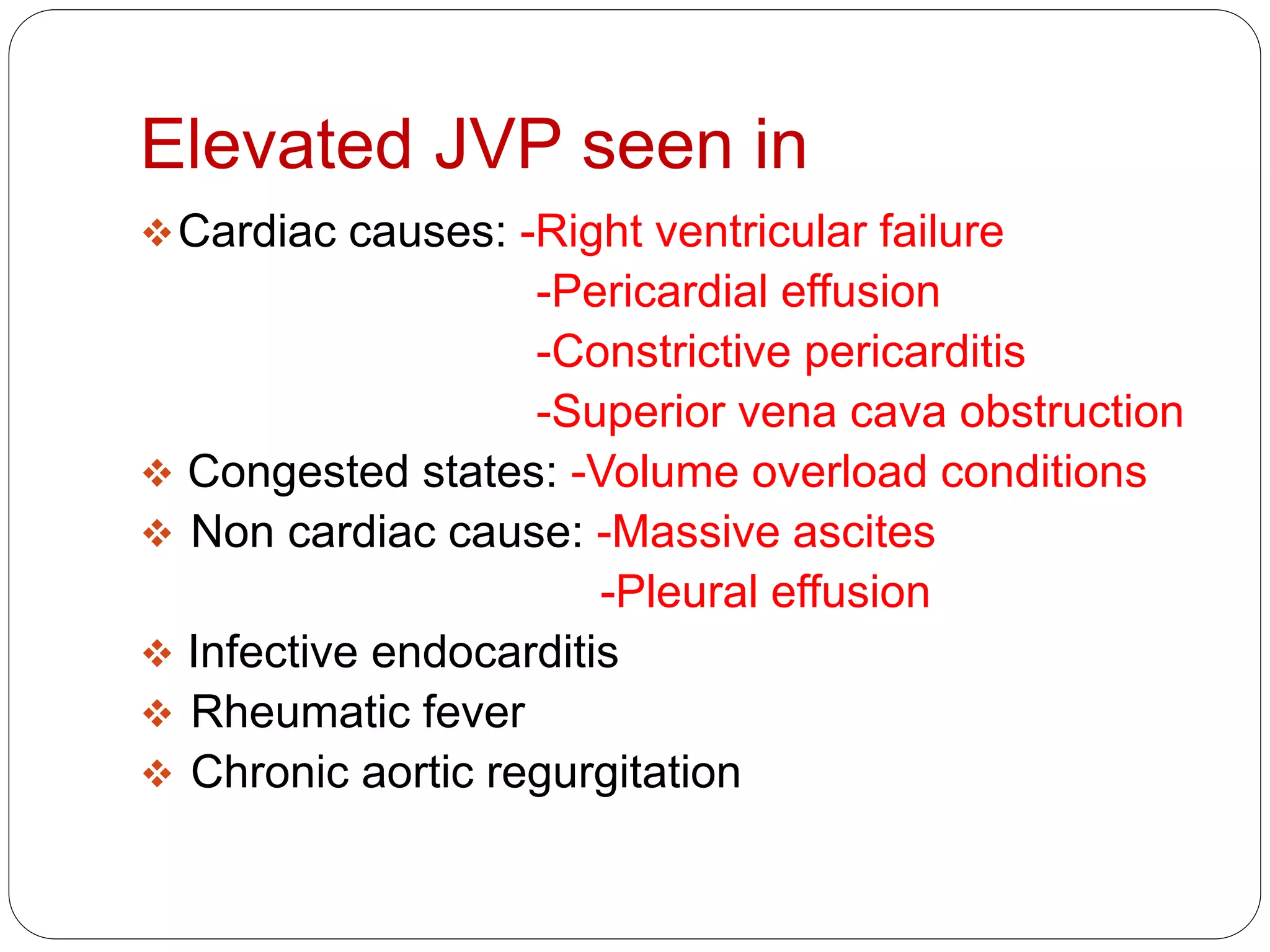
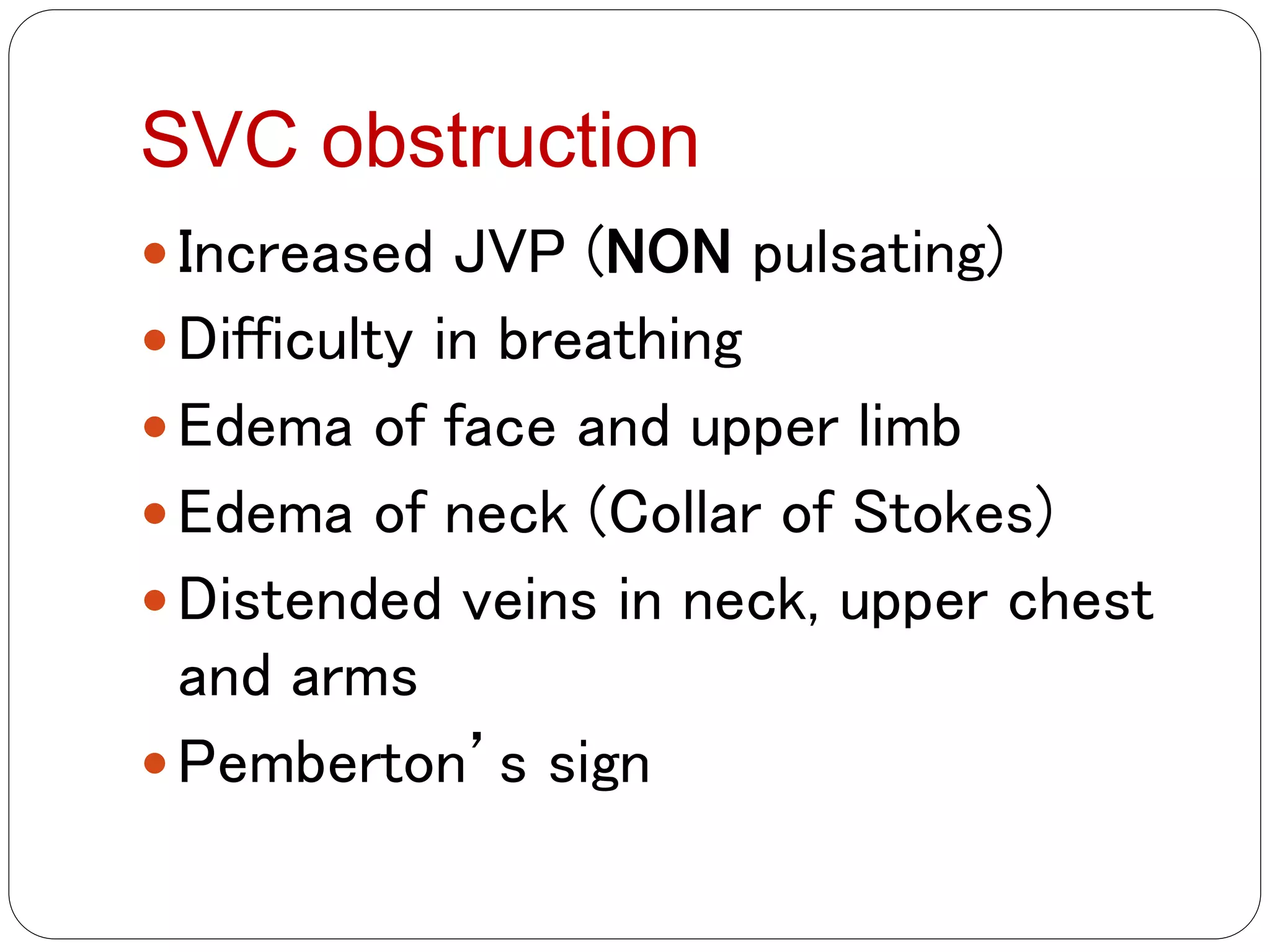
Elevated jugular venous pressure (JVP) can be caused by cardiac or non-cardiac conditions that increase right atrial pressure. A thorough history, physical exam including assessment of the jugular venous pulse, and initial tests are needed to differentiate between potential causes like heart failure, tricuspid valve disease, pulmonary embolism, pericardial effusion, or ascites. Initial management involves diuretics, further imaging like echocardiography, and sometimes invasive procedures to confirm the diagnosis and treat the underlying condition.