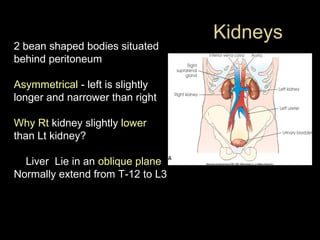
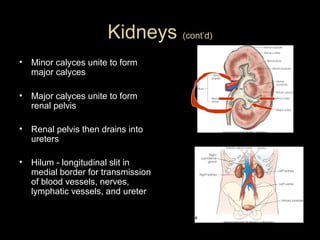
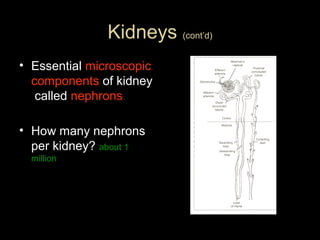
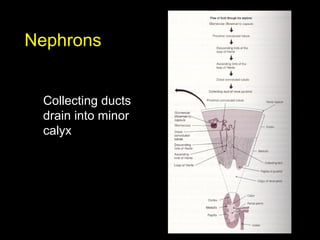
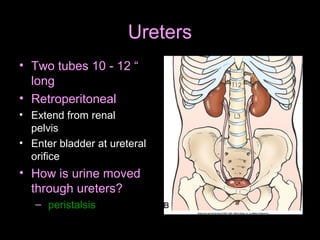
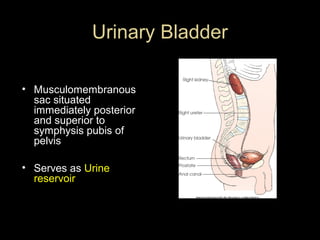
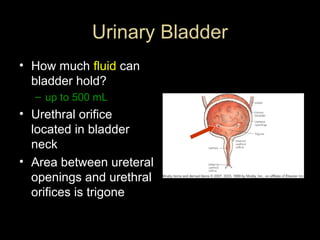
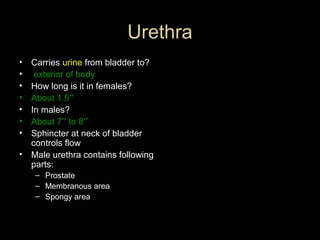
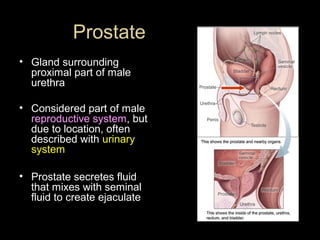
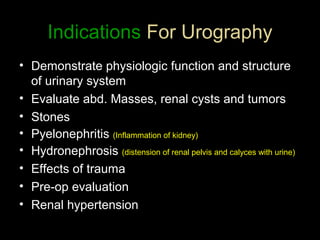
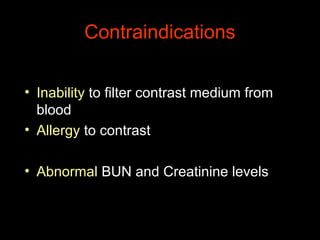
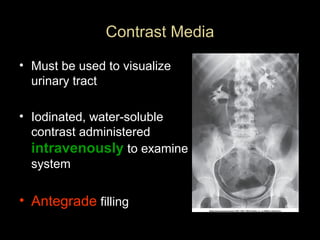
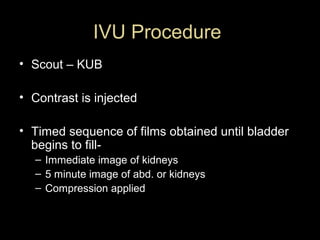
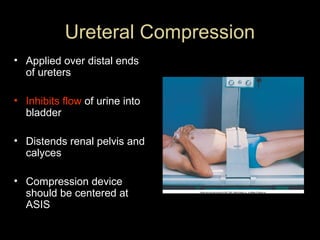
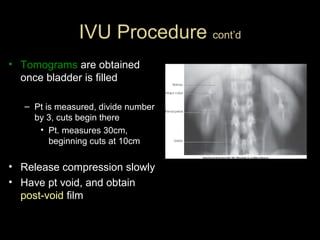
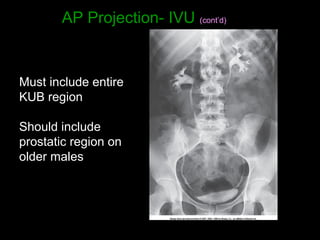
This document provides an overview of the urinary system including the kidneys, ureters, urinary bladder, and urethra. It describes the location and basic functions of the kidneys and notes they filter waste from the blood and help regulate fluid and electrolyte balance. The document also outlines the intravenous urogram procedure used to examine the urinary system including patient preparation, contrast injection, and obtaining radiographic images in multiple projections.