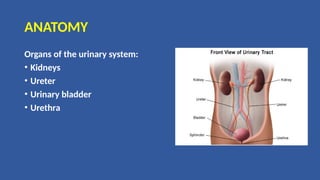
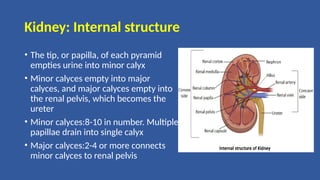
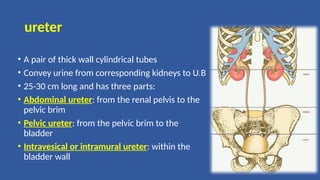
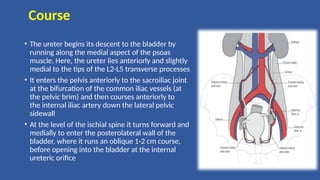
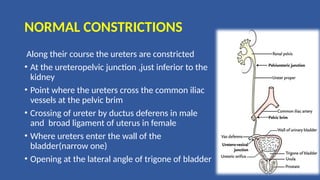
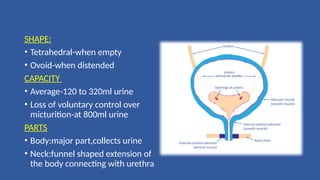
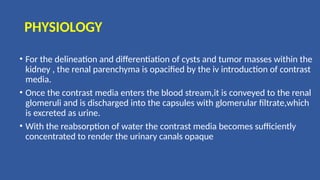
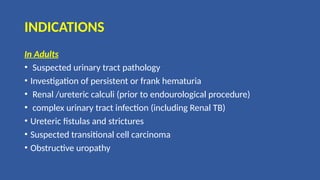
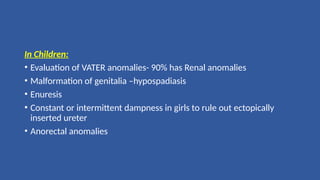
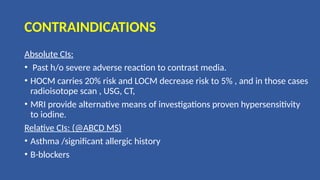
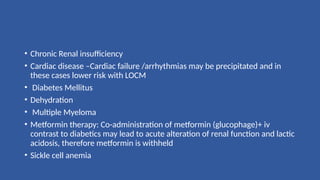
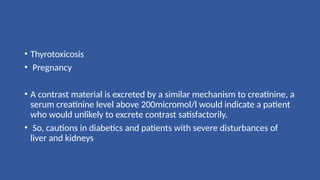
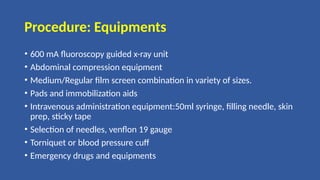
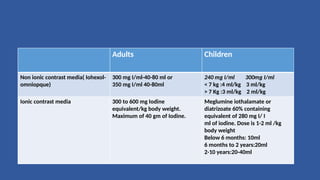
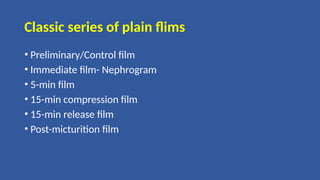
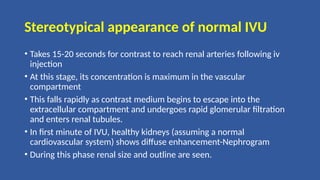
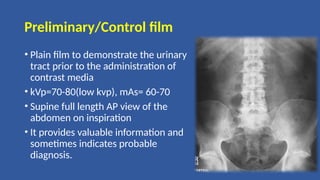
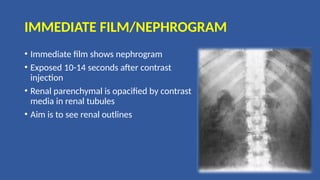
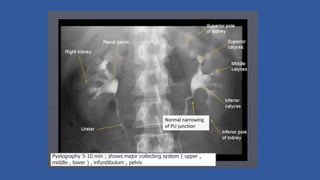
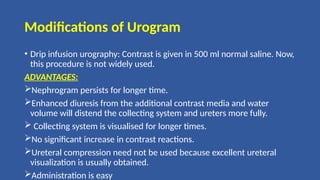
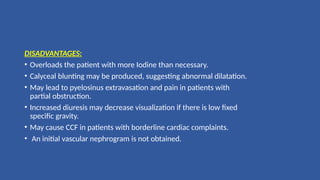
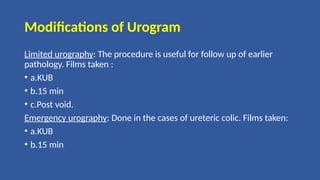
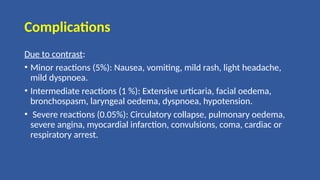
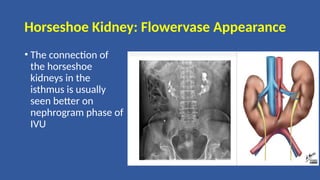
The document provides a comprehensive overview of intravenous urography (IVU), detailing its purpose, procedure, and the anatomy of the urinary system. It discusses the anatomical features of the kidneys, ureters, and bladder, alongside the methods and precautions involved in conducting the IVU test, including indications, contraindications, and patient preparation. Additionally, it outlines various imaging techniques during the procedure and the importance of contrast media in visualizing renal structures.