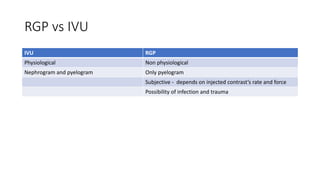
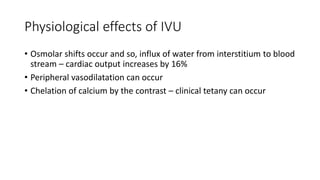
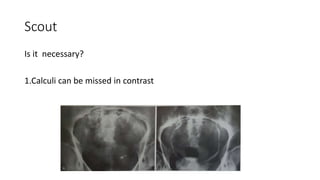
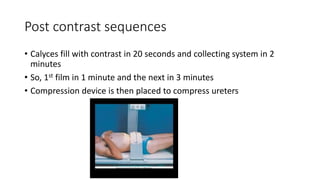
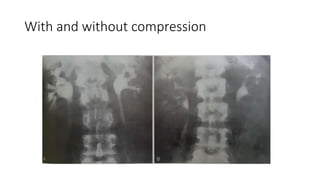
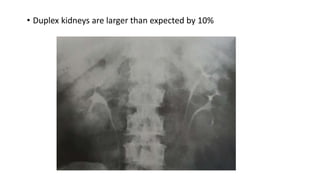
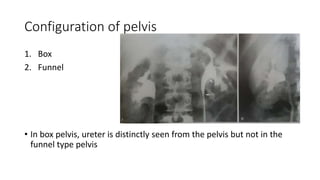
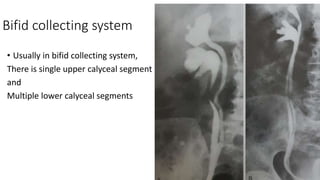
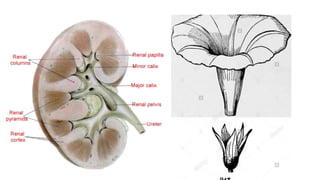
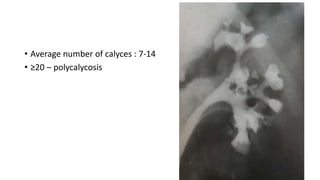
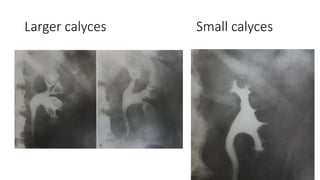
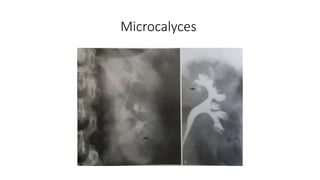
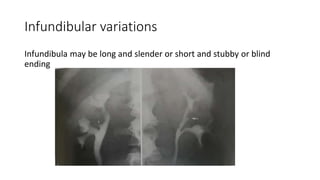
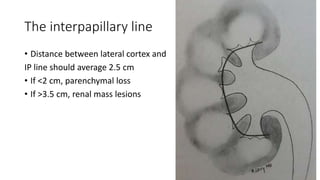
This document provides an overview of an intravenous urogram (IVU) procedure. It discusses the terminology, preparation of patients, technique and phases of an IVU, as well as the anatomy visualized through an IVU. Key points include: an IVU shows both nephrogram and pyelogram phases, while a retrograde pyelogram only shows the pyelogram; preparation such as catharsis and dehydration are no longer recommended; the technique involves contrast injection followed by imaging sequences at 1, 3, 10 and 20 minutes both supine and prone; and an IVU can visualize renal size, location, pelvis configuration, calyces, and ureteral anatomy.