This document provides an overview of intravenous urography (IVU), including indications, contraindications, risks, procedure details, and imaging techniques. Some key points:
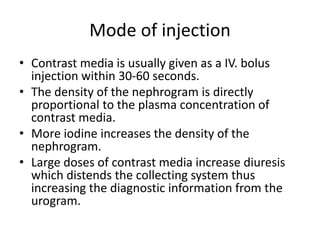
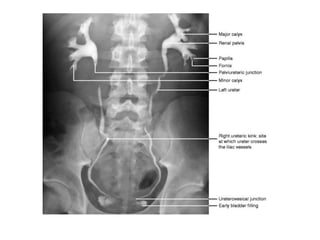
- IVU involves injecting contrast media intravenously to visualize the kidneys, ureters, and bladder. It is used to evaluate the entire urinary tract for various conditions like infections, abnormalities, and potential donors.
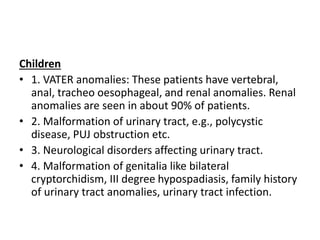
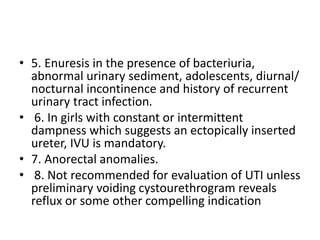
- Common indications include screening for hematuria, evaluating obstructive uropathy, and assessing renal anatomy in children with congenital anomalies.
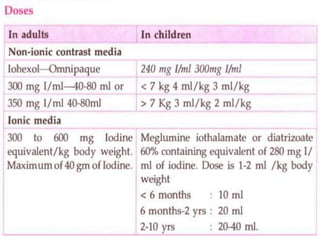
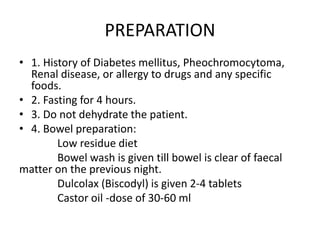
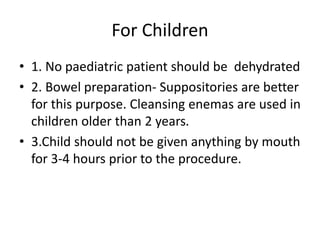
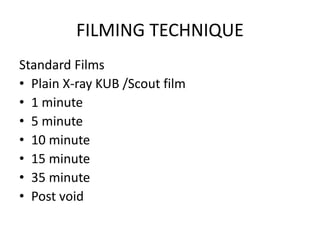
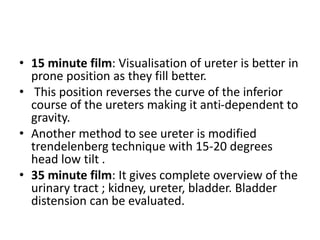
- Risks include allergic reactions. Preparation involves bowel cleansing and fasting prior. The procedure involves serial x-rays over 30-35 minutes to visualize contrast