This document discusses imaging of the urinary tract, including KUB (kidneys, ureters, bladder) radiography and intravenous urography (IVU). It provides details on:
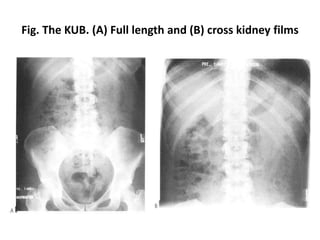
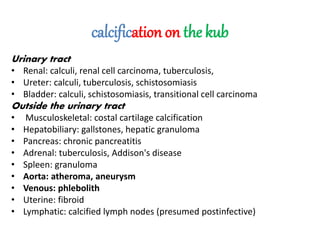
- The standard KUB technique using two abdominal x-ray images to outline the kidneys, ureters and bladder.
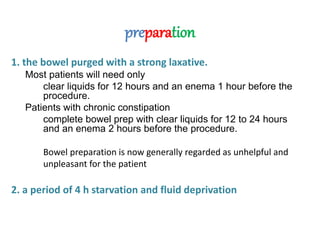
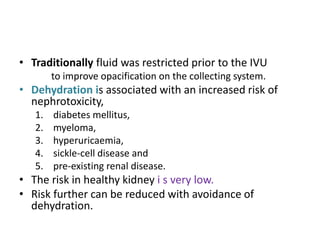
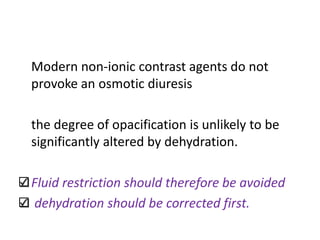
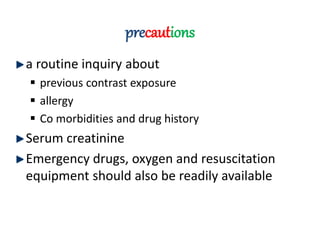
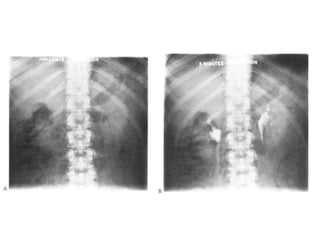
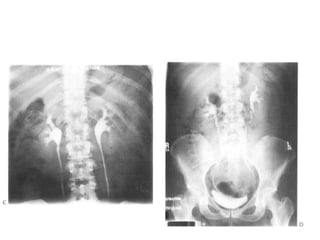
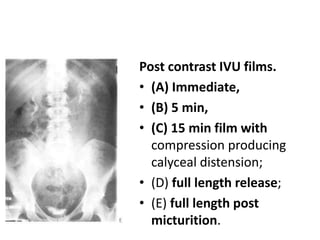
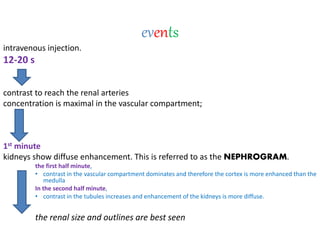
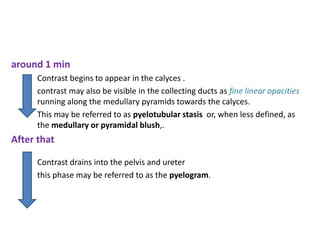
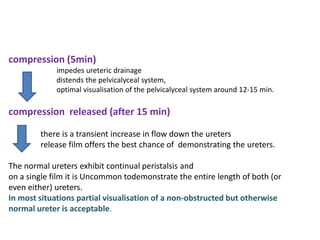
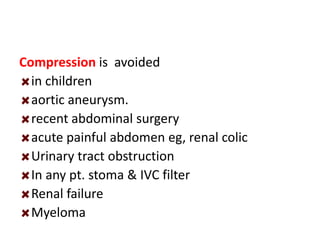
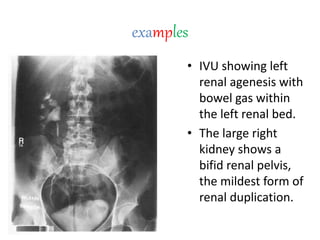
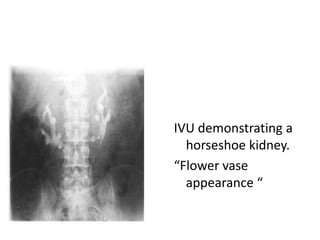
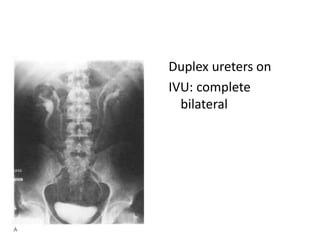
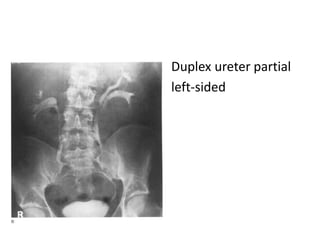
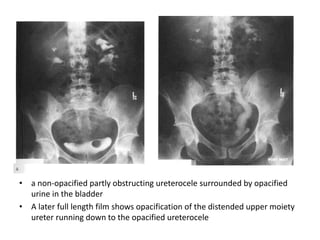
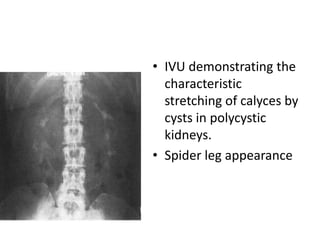
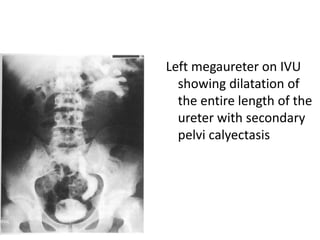
- The classic IVU procedure involving a series of x-ray images before and after intravenous injection of iodine contrast to visualize the functioning of the kidneys and urinary tract.
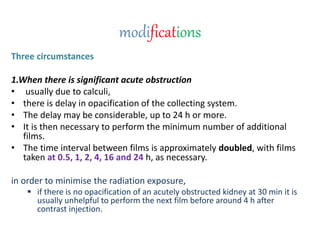
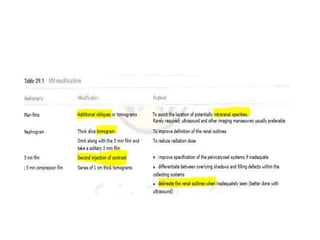
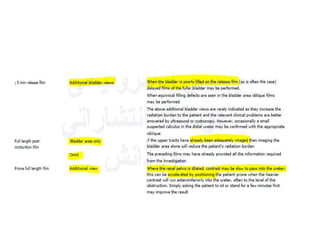
- Modifications of IVU for specific situations like urinary obstruction or pregnancy to minimize radiation exposure.