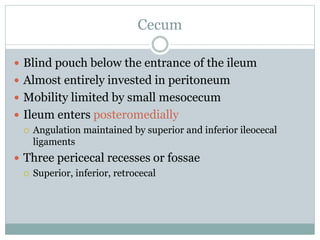
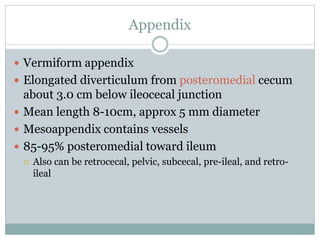
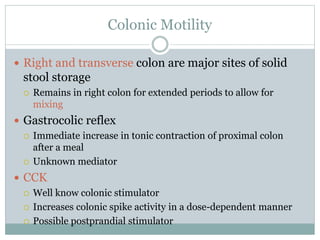
This document summarizes the anatomy and physiology of the colon. It describes the major sections of the colon including the cecum, appendix, ascending colon, transverse colon, descending colon, and sigmoid colon. It discusses the blood supply, innervation, motility, transport functions, and common conditions like constipation. In summary, it provides a comprehensive overview of the structure and functions of the colon.