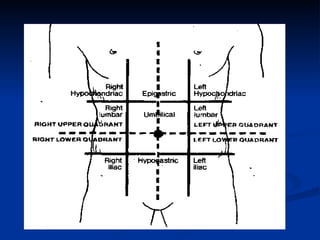
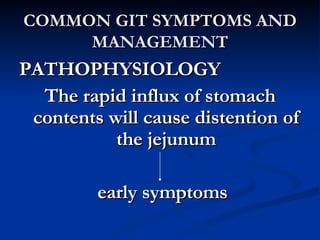
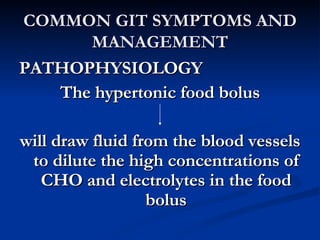
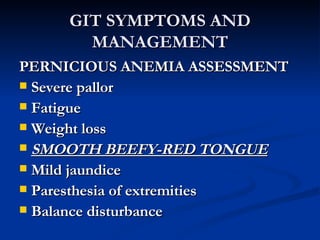
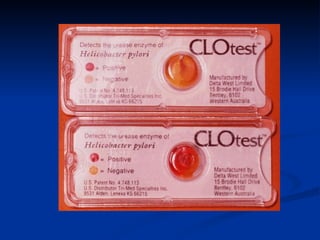
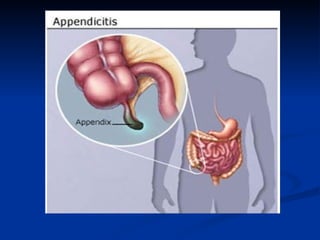
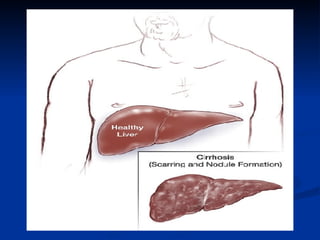
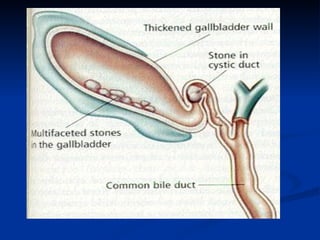
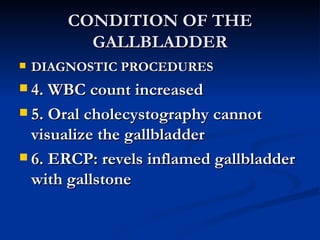
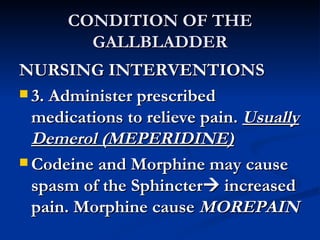
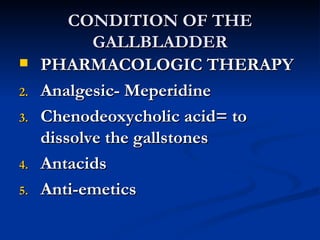
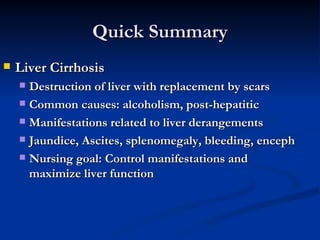
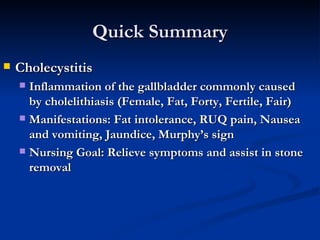
This document provides an overview of the anatomy and physiology of the gastrointestinal system and its components. It discusses the mouth, esophagus, stomach, small intestine, large intestine, liver, gallbladder and pancreas. It also reviews common laboratory procedures related to the GI system like fecalysis, upper and lower GI studies, and endoscopy. Common GI symptoms like constipation, diarrhea and dumping syndrome are discussed along with nursing interventions.