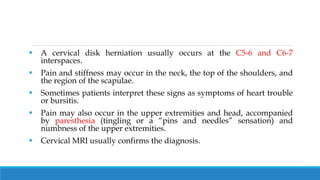
The document discusses cervical and lumbar disc herniation. It describes how cervical disc herniation typically occurs between the C5-C7 vertebrae and can cause neck and upper body pain. Medical management includes bed rest, cervical collars, traction and medications. Surgery may be required for significant issues. Lumbar disc herniation causes low back and leg pain. Medical management also focuses on bed rest, medications and heat. Surgery options include discectomy and newer minimally invasive techniques.




![PHARMACOLOGIC THERAPY
Analgesic agents (NSAIDs, propoxyphene [Darvon], oxycodone
[Tylox], or hydrocodone [Vicodin]) are prescribed during the acute
phase to relieve pain, and sedatives may be administered to control the
anxiety often associated with cervical disk disease.
Muscle relaxants (cyclobenzaprine [Flexeril], methocarbamol
[Robaxin], metaxalone [Skelaxin]) are administered to interrupt the
cycle of muscle spasm and to promote comfort.
NSAIDs (aspirin, ibuprofen [Motrin, Advil], naproxen [Naprosyn,
Anaprox]) or corticosteroids are prescribed to treat the inflammatory
response that usually occurs in the supporting tissues and affected
nerve roots.](https://image.slidesharecdn.com/intervertebraldischerniation-230202093850-123b19ef/85/Intervertebral-disc-herniation-pptx-7-320.jpg)





![SURGICAL MANAGEMENT
In the lumbar region, surgical treatment includes lumbar disk excision
through a postero lateral laminotomy and the newer techniques of
micro-discectomy and percutaneous discectomy.
In microdiscectomy, an operating microscope is used to visualize the
offending disk and compressed nerve roots; it permits a small
incision(2.5 cm [1 inch]) and minimal blood loss and takes about 30
minutes of operating time.
Generally, it involves a short hospital stay, and the patient makes a
rapid recovery.](https://image.slidesharecdn.com/intervertebraldischerniation-230202093850-123b19ef/85/Intervertebral-disc-herniation-pptx-17-320.jpg)