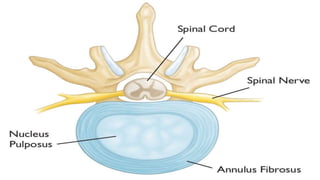
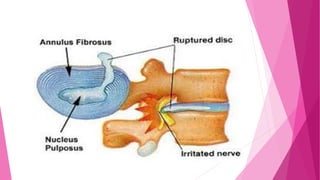
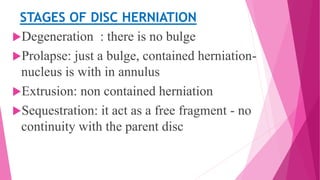
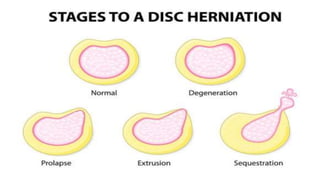
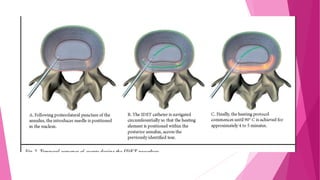
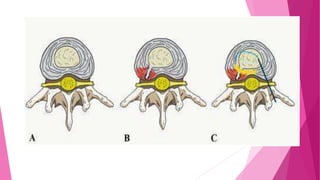
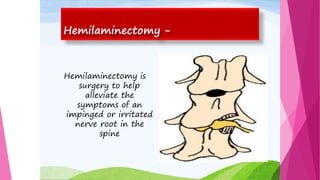
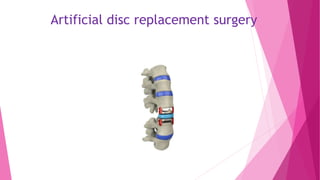
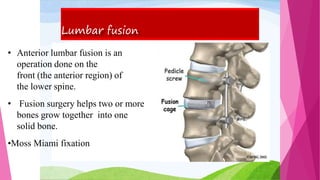
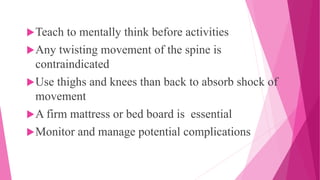
Intervertebral disc prolapse (IVDP) is a condition involving the degeneration and herniation of intervertebral discs, which can lead to symptoms like pain, numbness, and muscle weakness depending on its location. Management includes medical treatment, physical therapy, and possibly surgical intervention if conservative methods fail. Assessment and nursing care focus on pain relief, monitoring for complications, and promoting mobility post-surgery.