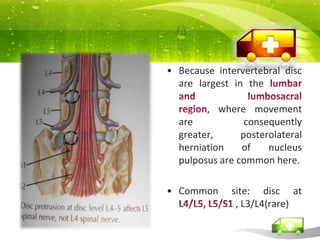
1. Prolapsed intervertebral disc occurs when the gelatinous nucleus pulposus squeezes through the annulus fibrosus and bulges posteriorly or laterally, commonly compressing spinal nerves.
2. Spinal stenosis is a narrowing of the spinal canal that results in cord or root compression. It is often caused by degenerative changes like osteophyte formation.
3. Spondylosis, or spinal osteoarthritis, involves degenerative changes in discs, facets, and joints that cause loss of normal spinal structure and function, commonly affecting the cervical, thoracic, or lumbar regions.