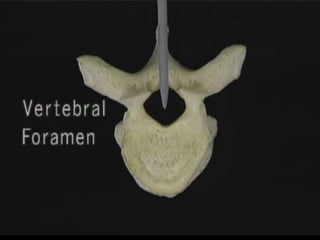
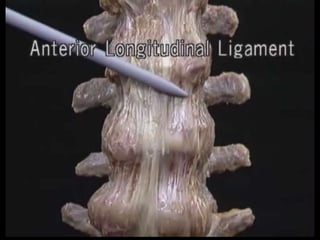
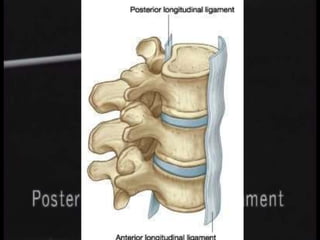
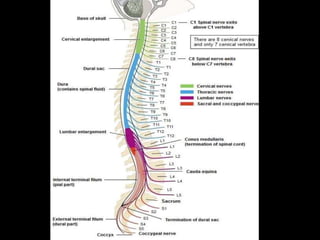
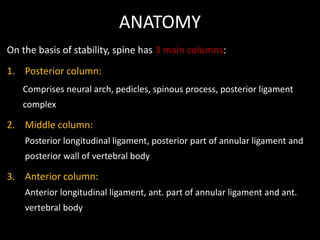
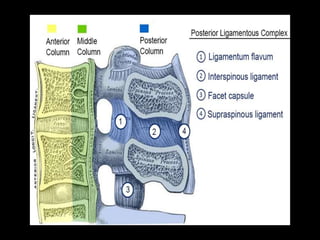
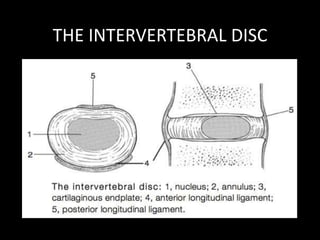
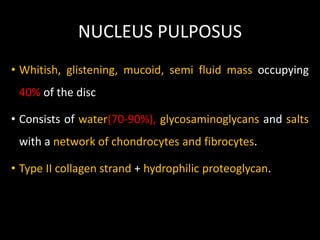
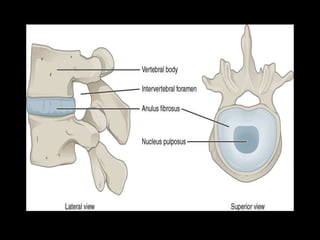
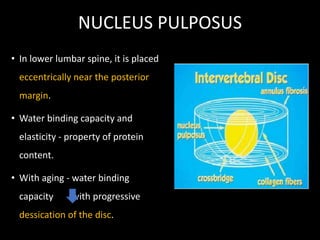
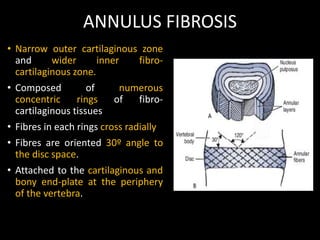
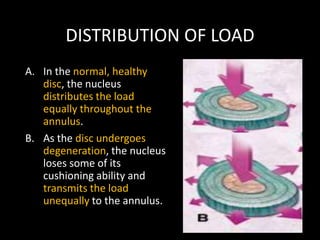
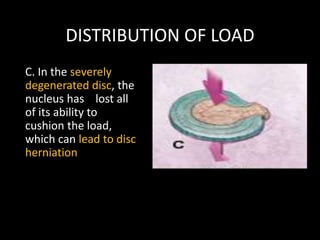
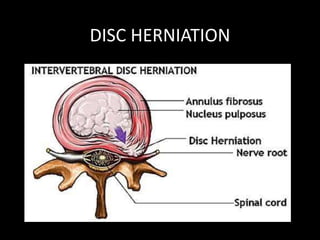
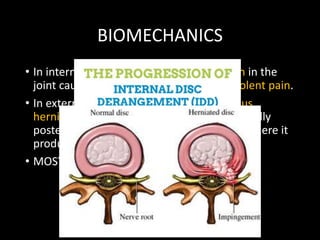
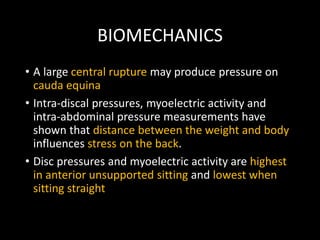
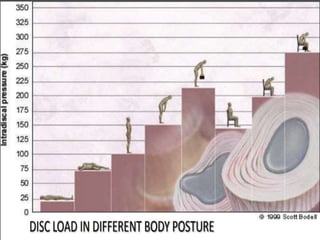
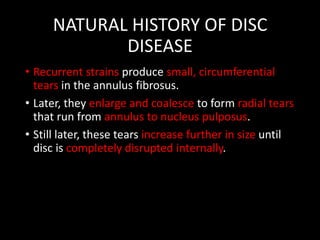
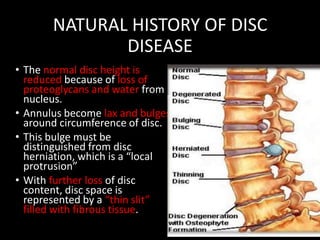
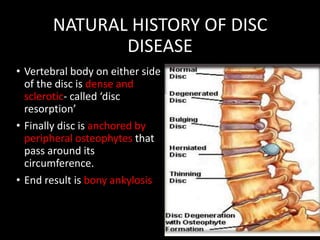
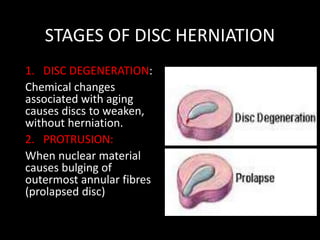
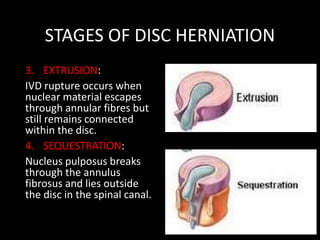
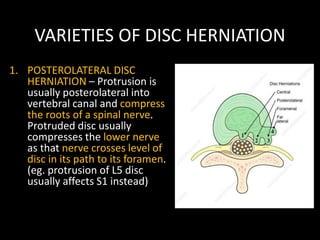
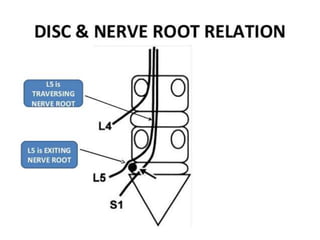
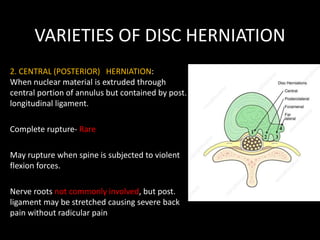
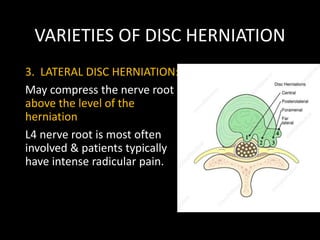
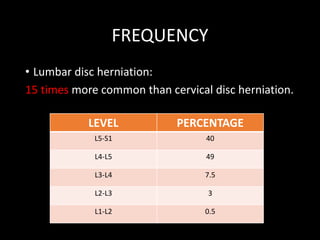
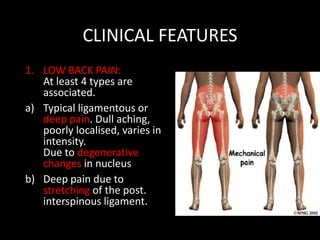
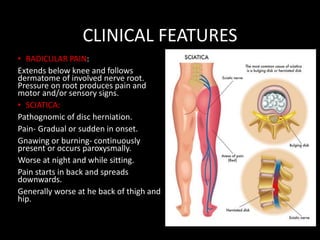
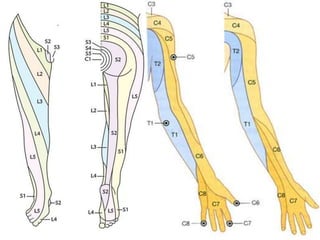
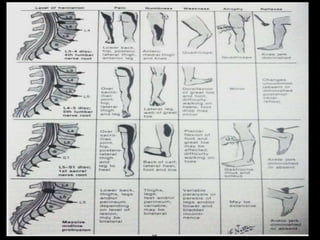
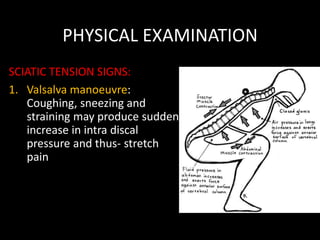
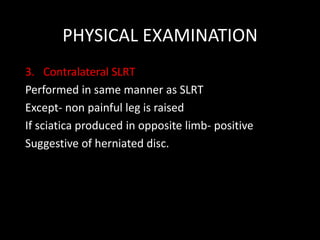
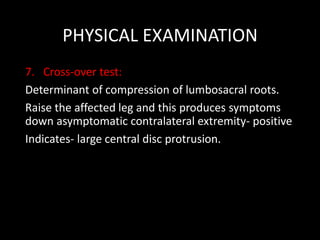
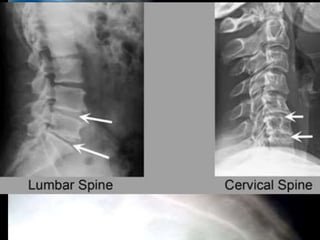
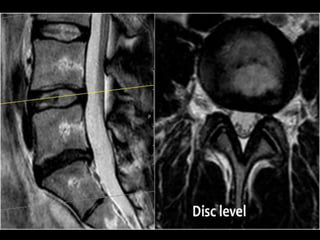
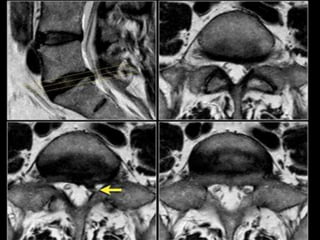
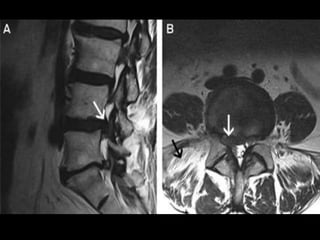
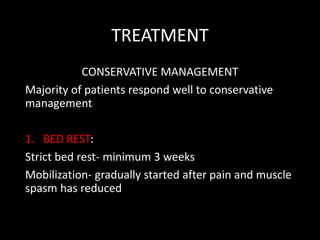
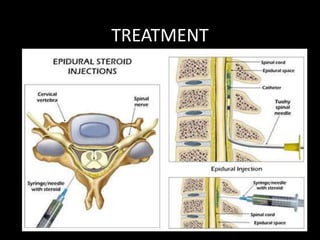
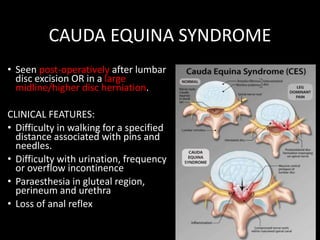
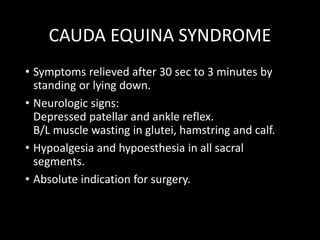
The document provides a comprehensive overview of prolapsed intervertebral disc (PIVD), detailing its definition, history, anatomy, functions, herniation types, and associated clinical features. It outlines the causes, implications of degeneration, various tests for diagnosis, and common forms of disc herniation, particularly in the lumbar and cervical regions. The document also emphasizes the importance of mechanical factors, lifestyle impacts, and specific symptoms linked to PIVD for proper identification and treatment.