1) Inguinal hernias are common, with approximately 700,000 repairs performed annually in the US, mostly occurring in males.
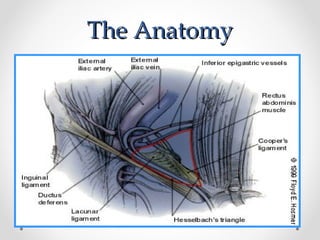
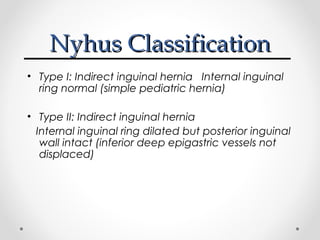
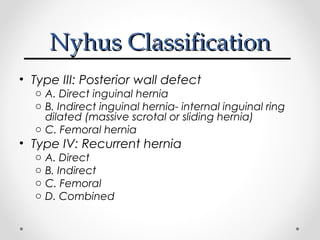
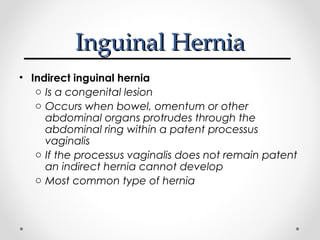
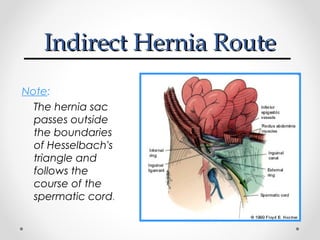
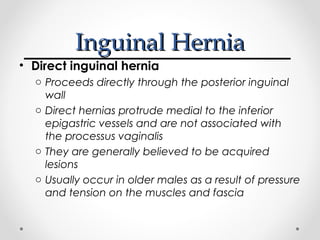
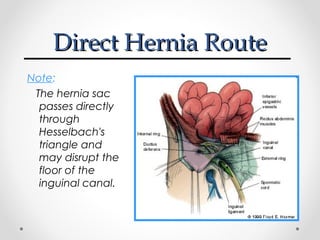
2) There are two main types of inguinal hernias - indirect and direct. Indirect hernias are congenital while direct hernias are acquired lesions that occur through the posterior inguinal wall.
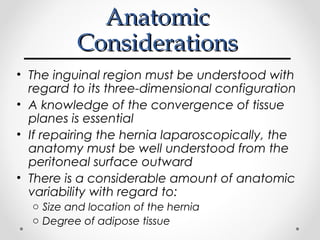
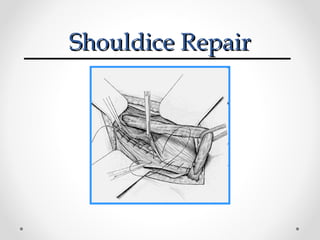
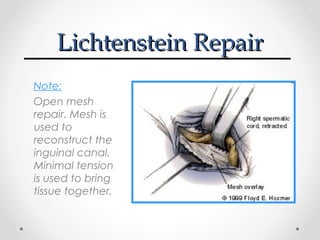
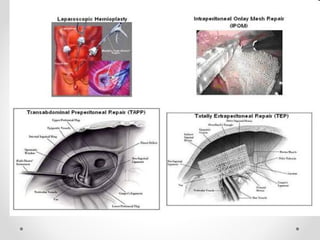
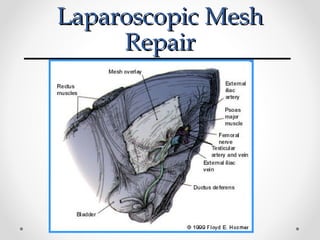
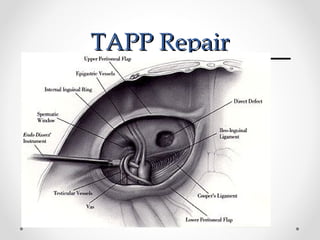
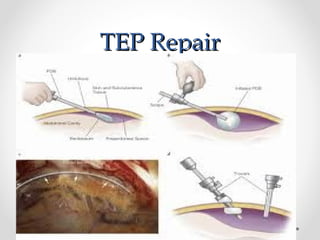
3) Common surgical repair options include the Lichtenstein tension-free repair using mesh, the Shouldice repair with overlapping tissue layers, and laparoscopic repairs like TAPP and TEP which utilize a mesh placed laparoscopically.