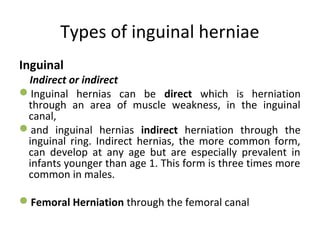
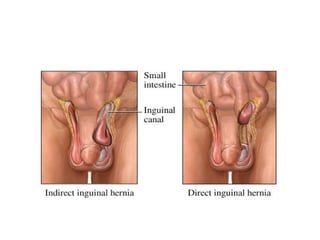
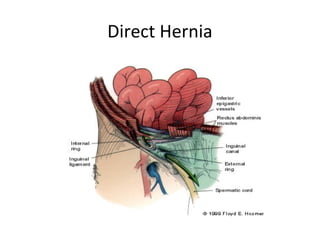
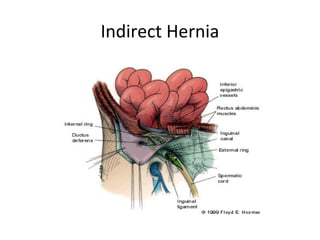
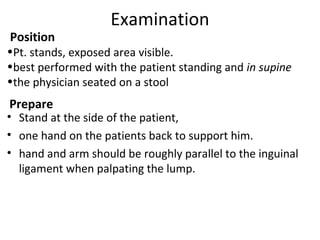
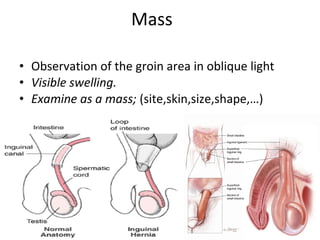
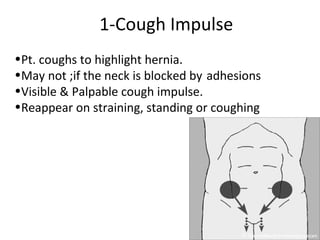
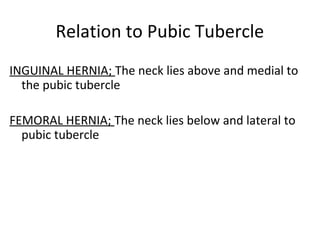
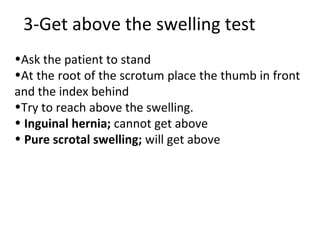
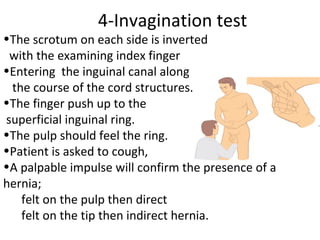
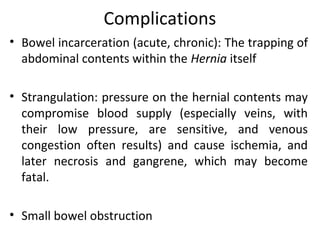
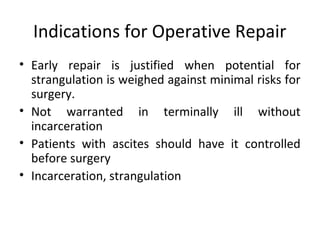
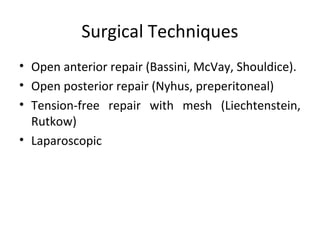
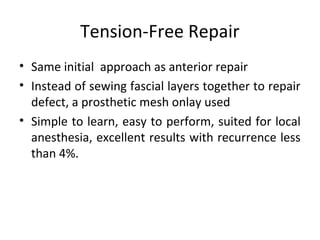
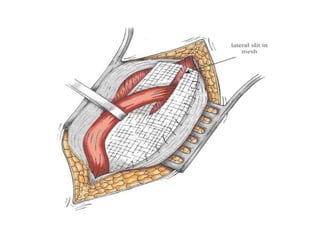
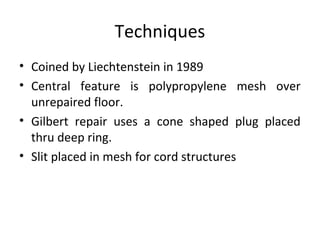
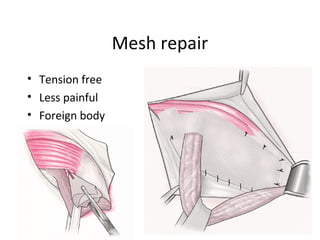
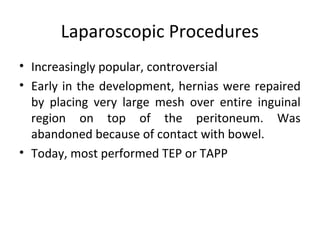
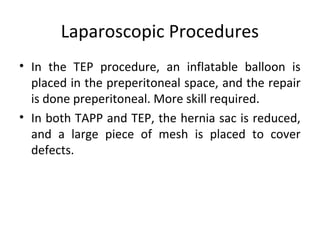
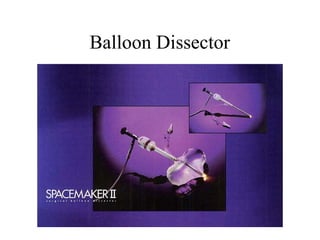
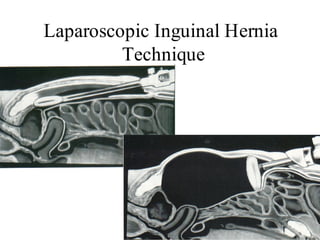
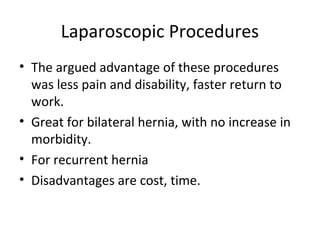
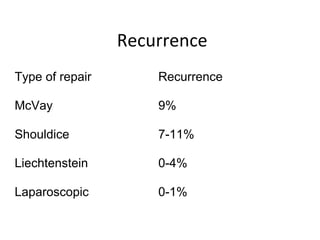
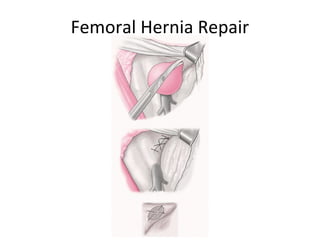
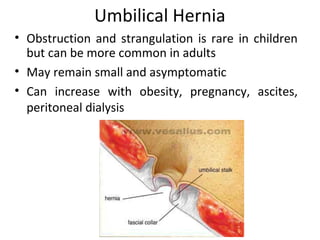
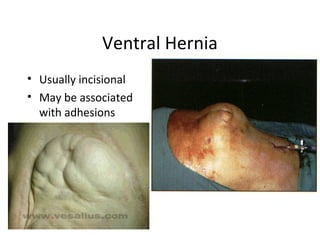
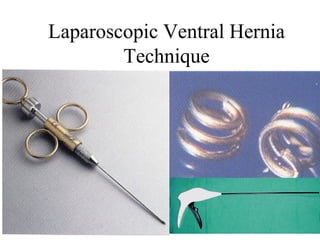
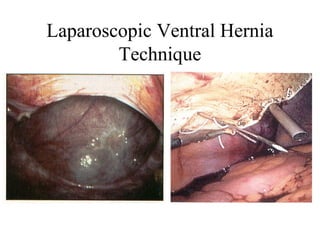
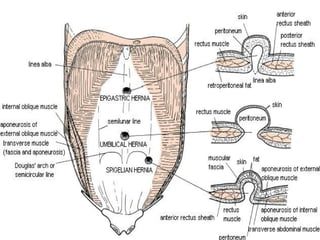
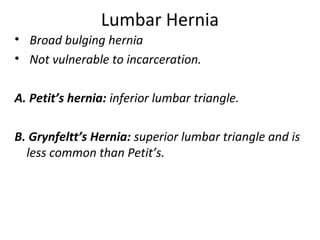
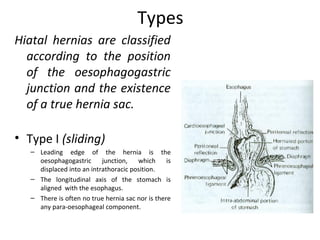
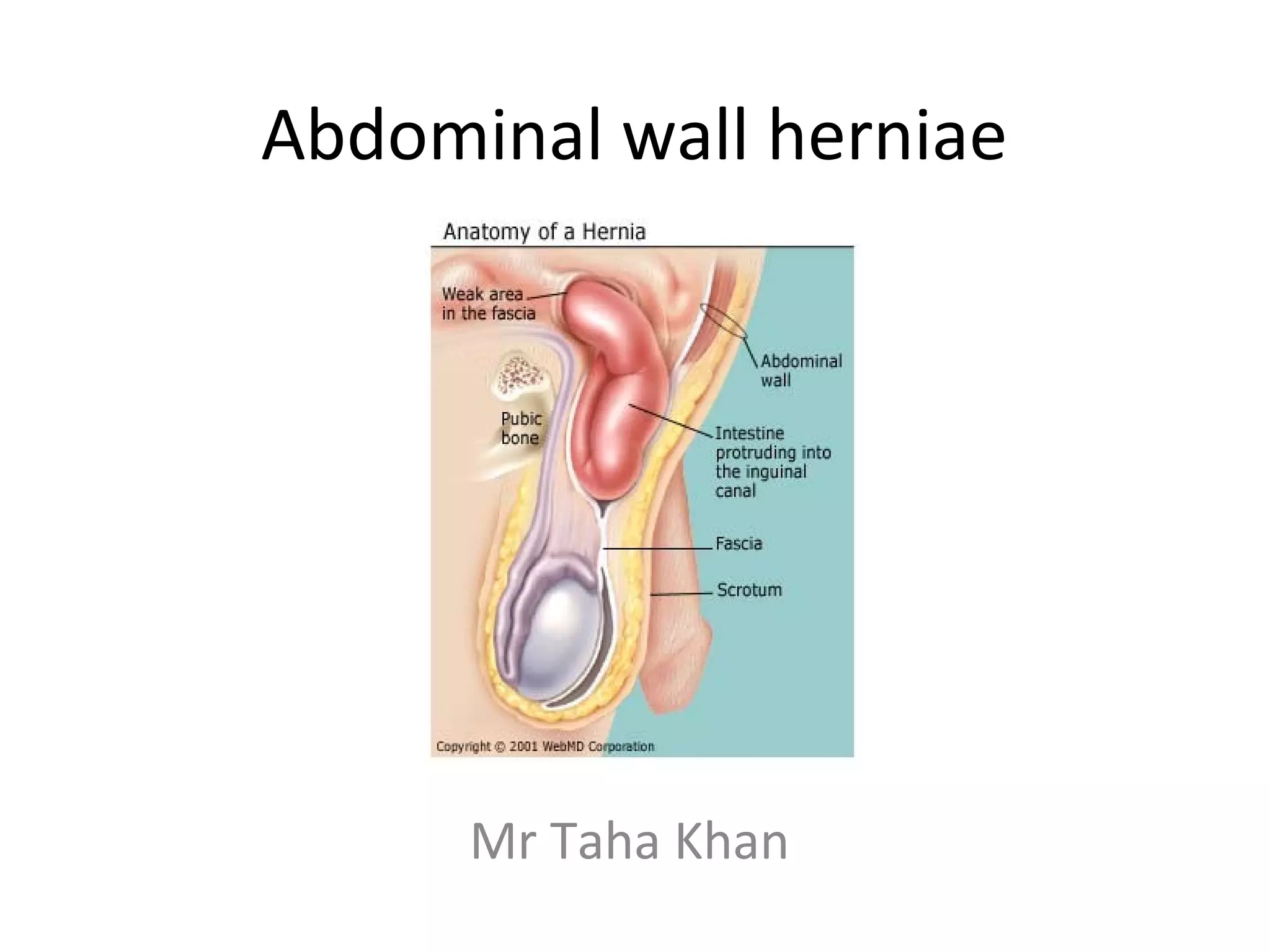
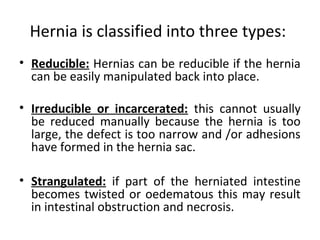
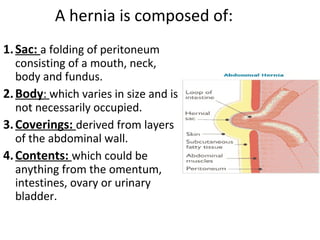
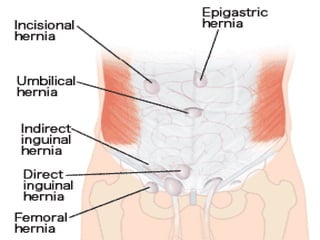
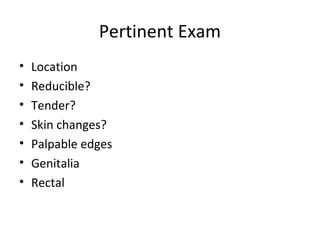
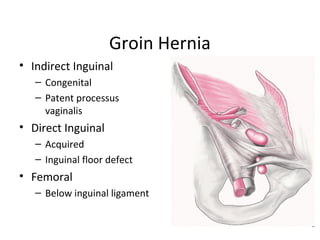
Abdominal wall herniae are classified as reducible, irreducible, or strangulated. Hernias contain a sac protruding through a defect in the abdominal wall and may contain organs like the intestines, omentum, or bladder. Common hernia types are inguinal, femoral, umbilical, incisional, and hiatal. A hernia exam evaluates for cough impulse, reducibility, location above the pubic tubercle, and differentiates direct from indirect inguinal hernias. Surgical repair techniques include open anterior and posterior approaches, tension-free repairs using mesh, and laparoscopic procedures. Complications include incarceration, strangulation, recurrence, infection, and nerve damage
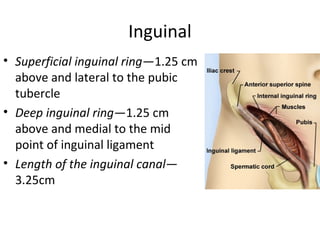
![Ingiunal canal Boundaries
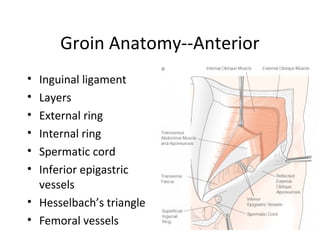
MALT: 2M 2A, 2L, 2T:
Superior wall [roof]: 2 Muscles:
• Internal oblique Muscle
• Transverse abdominus Muscle
Anterior wall: 2 Aponeuroses:
• Aponeurosis of external oblique
• Aponeurosis of internal oblique
Lower wall [floor]: 2 Ligaments:
• Inguinal Ligament
• Lacunar Ligament
Posterior wall: 2Ts:
• Transversalis fascia [laterally]
• Conjoint Tendon [medially]](https://image.slidesharecdn.com/abdominalwallherniae-130518052821-phpapp02/85/Abdominal-wall-herniae-17-320.jpg)