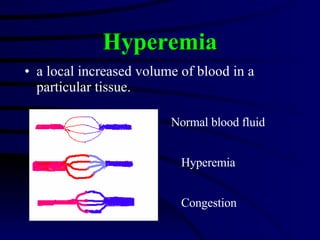
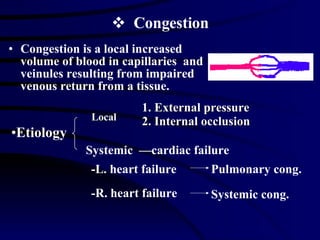
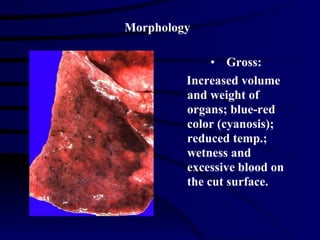
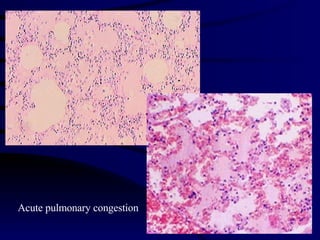
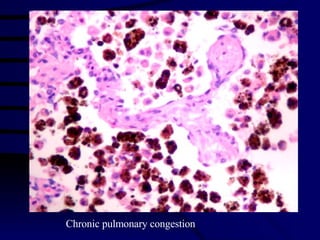
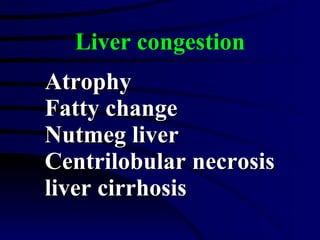
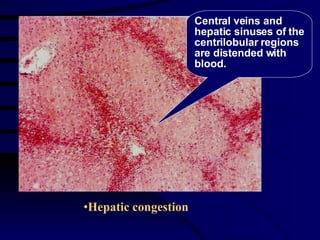
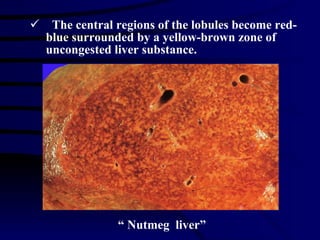
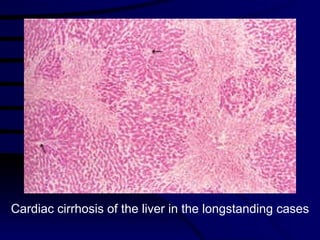
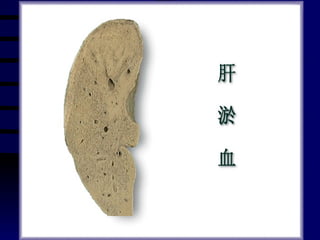
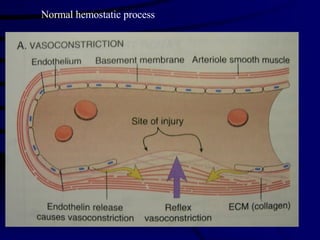
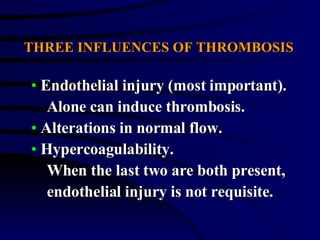
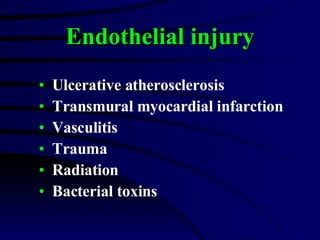
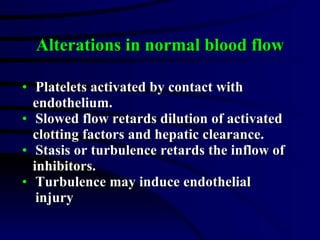
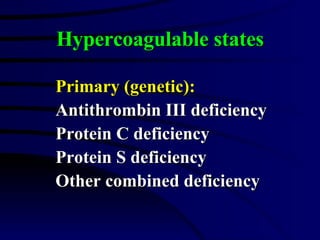
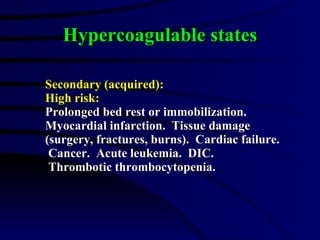
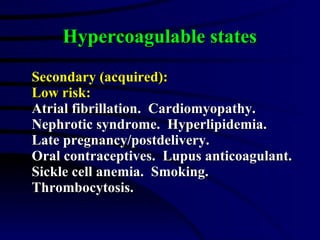
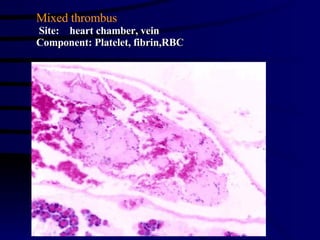
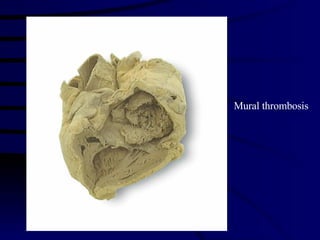
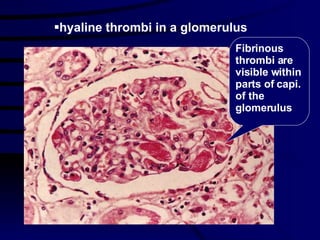
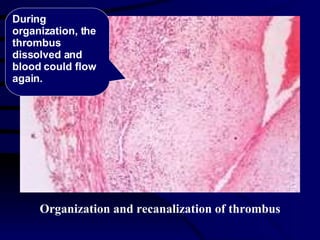
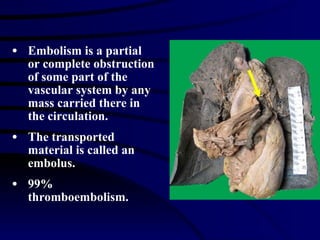
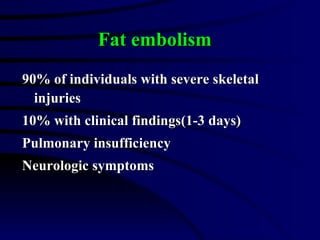
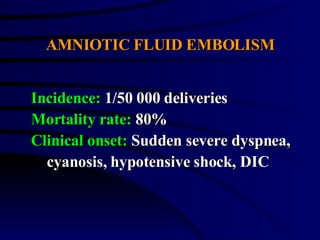
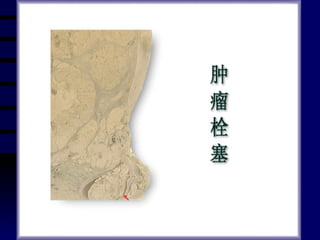
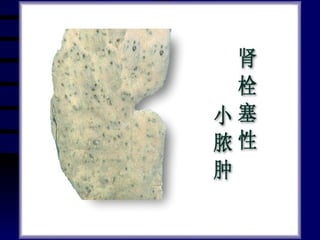
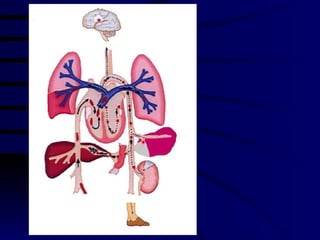
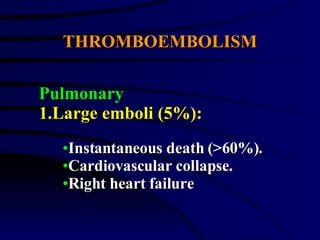
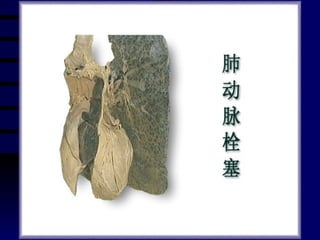
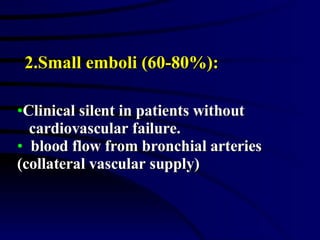
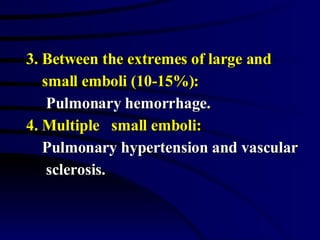
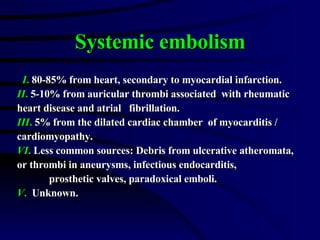
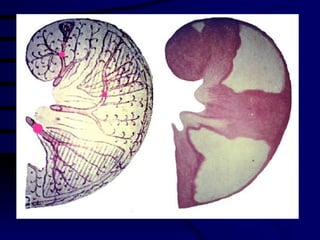
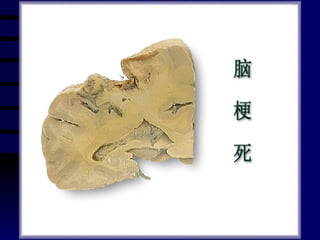
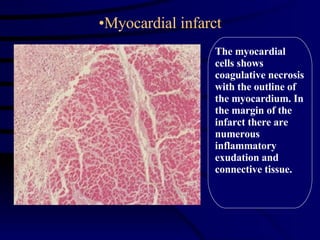
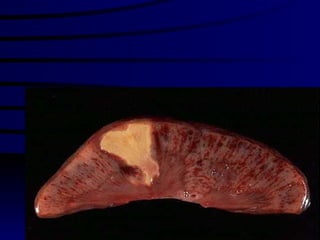
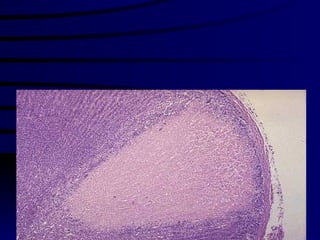
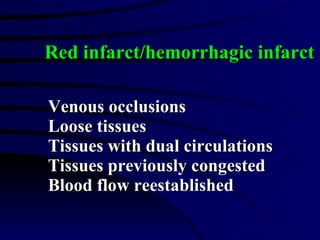
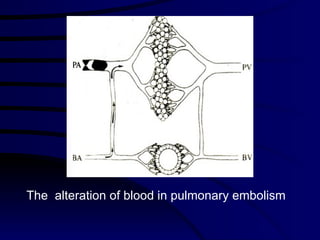
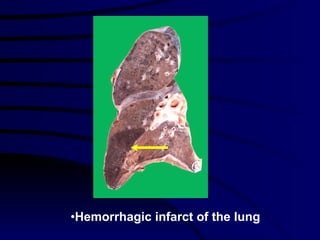
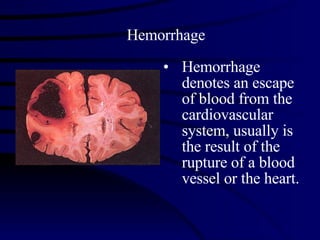
The document discusses various hemodynamic disorders including hyperemia, congestion, thrombosis, embolism, and infarction. Hyperemia is an increased blood volume in tissue from vasodilation. Congestion is increased blood volume from impaired venous return. Thrombosis is the formation of a blood clot within vessels. An embolism occurs when a piece of thrombus or other material blocks a vessel. Infarction is tissue death from blocked arteries or veins.