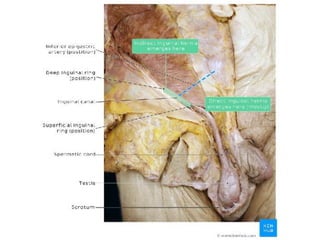
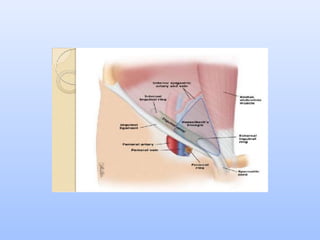
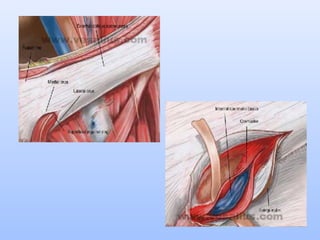
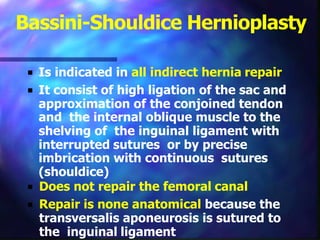
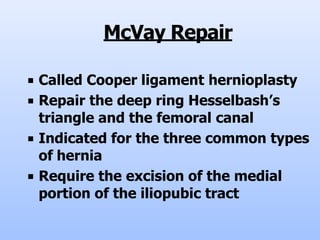
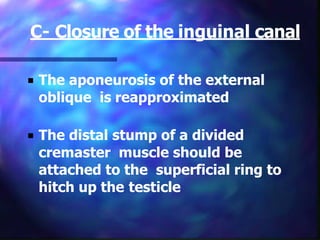
A hernia is a protrusion of an organ or tissue through a weakness in the wall of the cavity that normally contains it. There are several types of abdominal hernias classified by location, including inguinal, femoral, umbilical, and incisional hernias. Management of hernias involves both non-surgical and surgical options. Surgical repairs aim to reinforce or reconstruct the weakened abdominal wall using both open and laparoscopic techniques with mesh placement. Complications can include hemorrhage, infection, nerve injury, and hernia recurrence if tension is not adequately relieved during the repair.