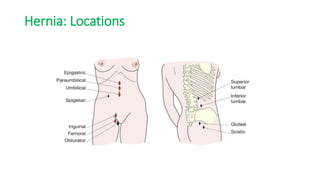
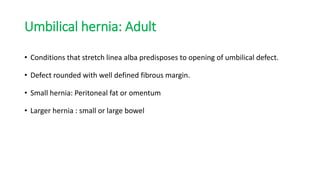
Ventral hernias occur when abdominal contents protrude through weaknesses in the abdominal wall. There are several types of ventral hernias classified by location and complexity. Examination involves evaluating for reducibility, tenderness, and signs of incarceration or strangulation. Treatment often involves surgical repair using sutures or mesh placement to reinforce the defect. Laparoscopic and open approaches are options depending on hernia characteristics.