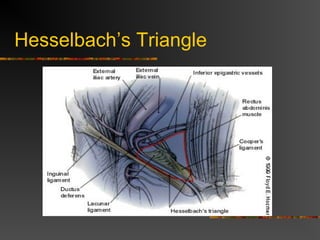
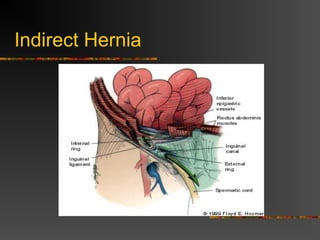
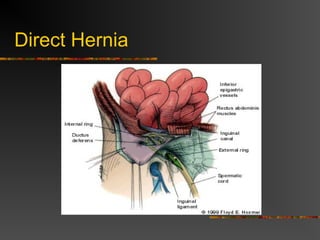
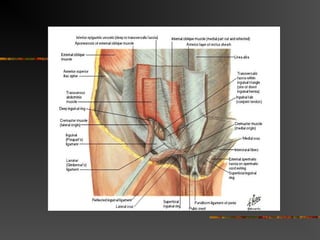
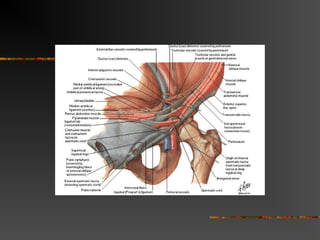
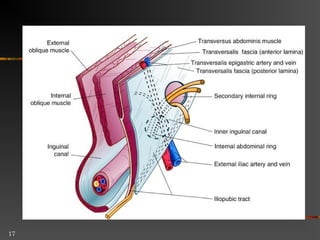
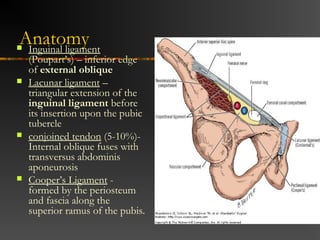
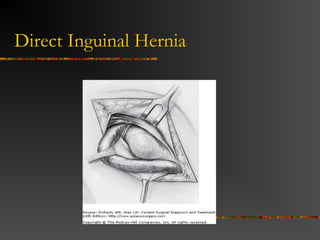
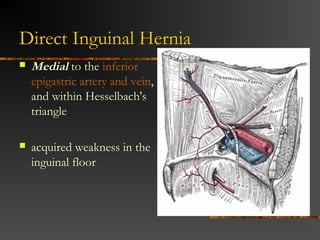
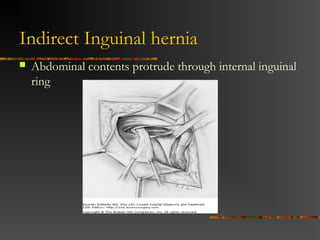
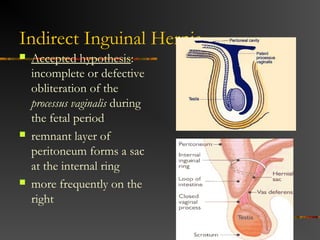
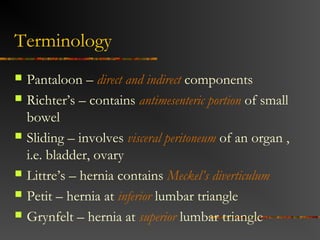
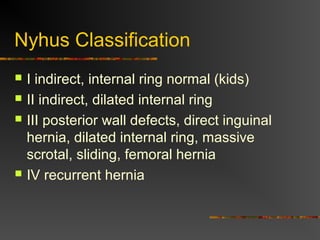
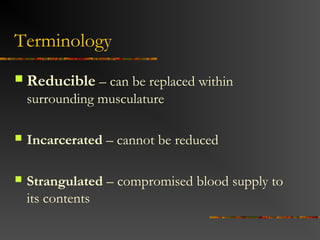
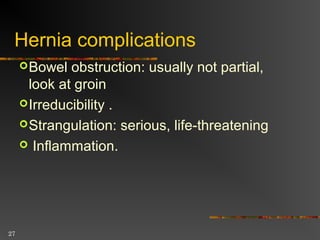
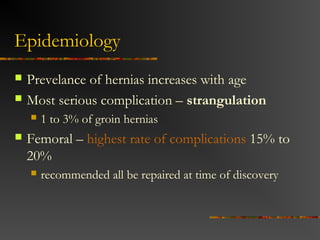
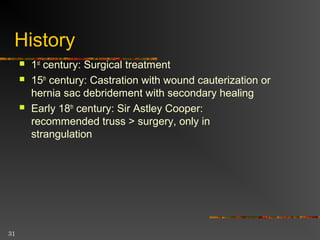
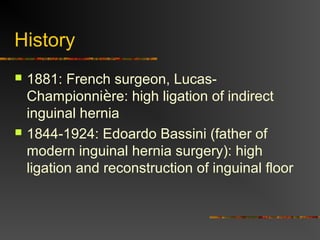
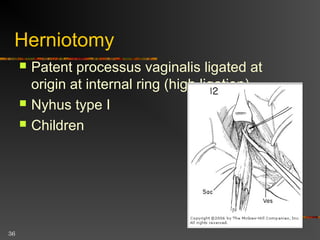
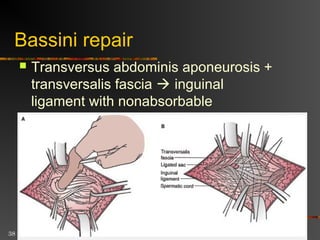
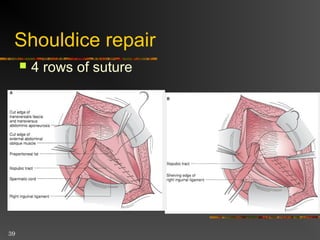
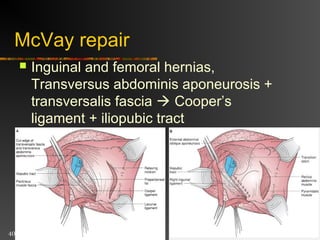
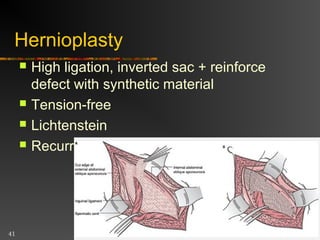
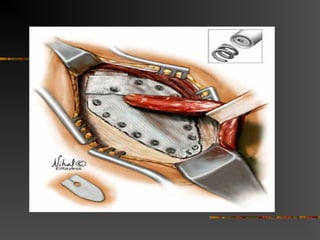
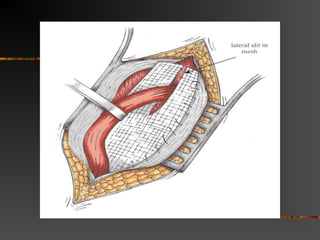
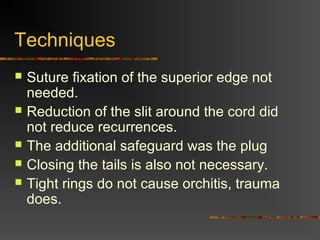
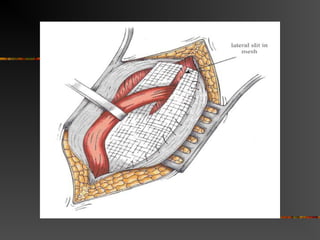
This document discusses groin hernias, including their definition, anatomy, types, and treatment methods. It notes that inguinal hernias are most common, occurring in 96% of cases, and are more frequent in males. The two main types are indirect hernias, which pass through the internal ring, and direct hernias, which occur through Hesselbach's triangle. Treatment has evolved from early cauterization and debridement to modern tension-free repairs using synthetic mesh, which have significantly lower recurrence rates than open suture repairs. Laparoscopic techniques are increasingly utilized but remain more complex and costly.