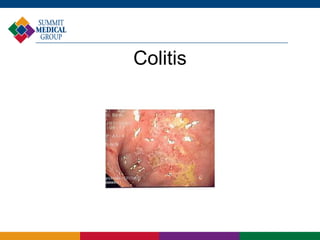
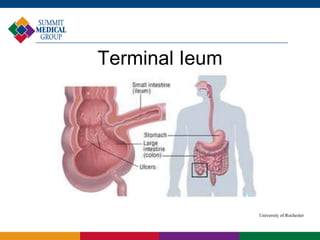
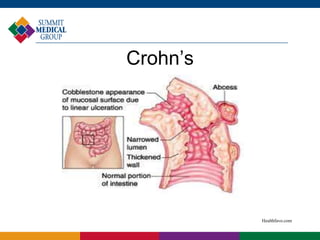
Inflammatory bowel disease encompasses ulcerative colitis and Crohn's disease, affecting approximately 1.4 million people in the U.S. These chronic conditions involve immune-mediated inflammation of the gastrointestinal tract, with distinct characteristics and treatment options. While there is no cure, effective treatments allow many patients to achieve remission and maintain a normal life.