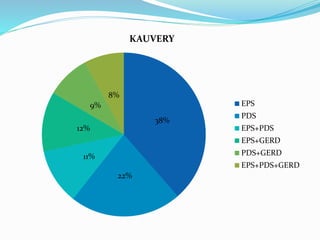
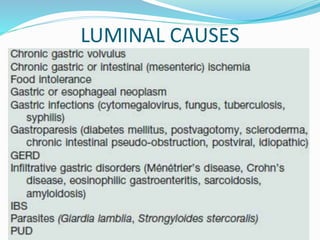
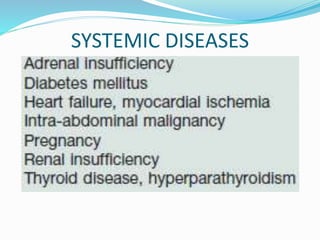
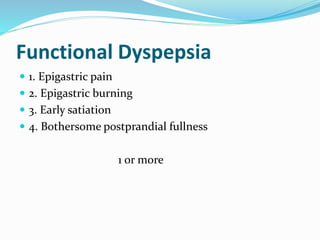
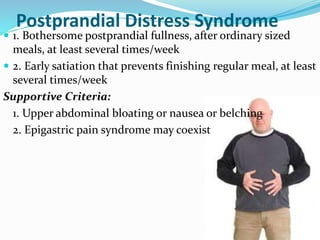
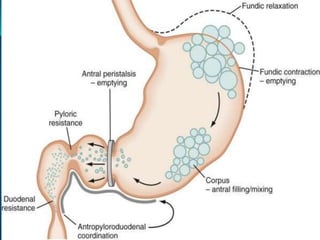
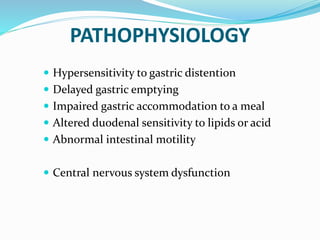
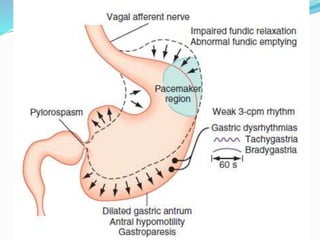
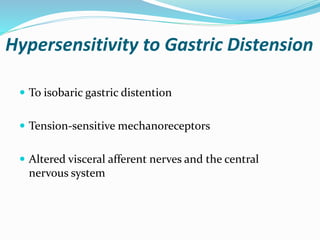
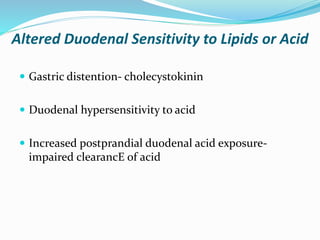
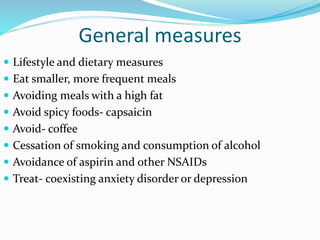
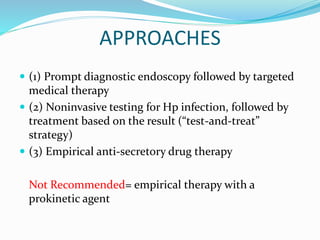
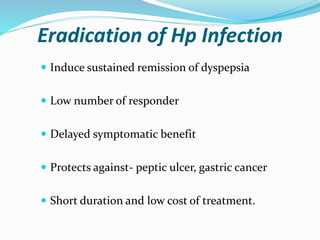
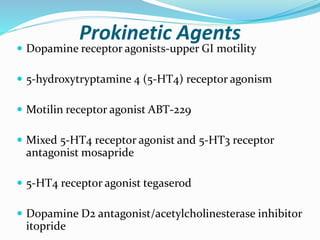
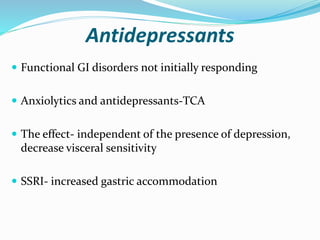
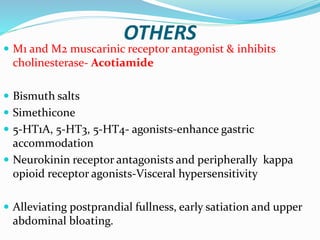
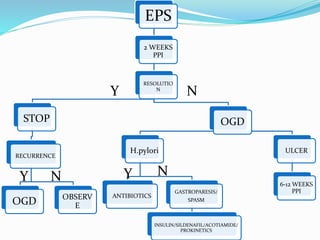
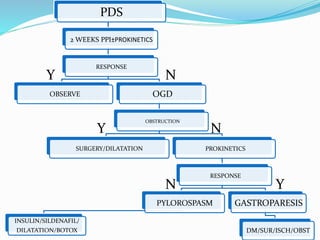
Dyspepsia refers to pain or discomfort centered in the upper abdomen. It is a common symptom with various potential causes. The document discusses the definitions, epidemiology, evaluation, and management approaches for different types of dyspepsia including functional dyspepsia and its subtypes of epigastric pain syndrome and postprandial distress syndrome. Testing and treatment are targeted based on alarm features and potential underlying causes, with a focus on lifestyle changes, antisecretory drugs, H. pylori treatment, prokinetics, and other pharmacological and psychological interventions.