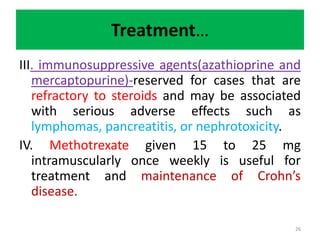
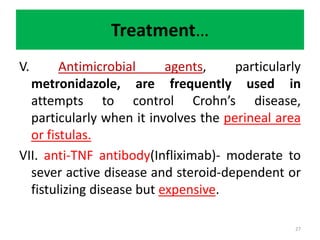
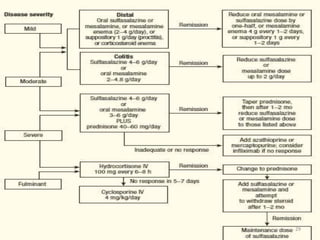
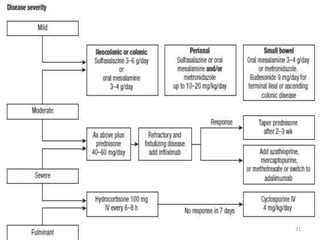
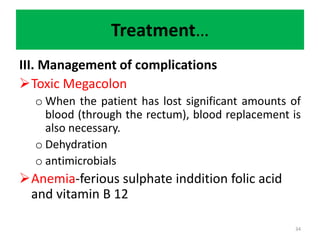
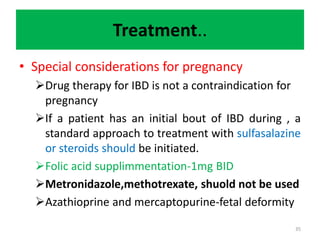
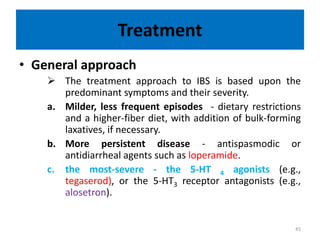
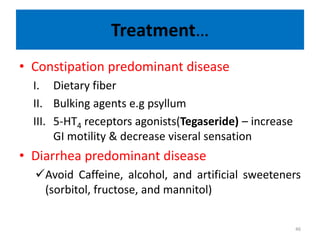
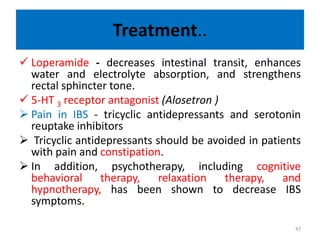
This document provides an overview of the pharmacotherapy of inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). It defines IBD and IBS, discusses their pathophysiology and clinical presentation. For treatment, it outlines the general approaches including medications used to induce and maintain remission for IBD such as aminosalicylates, corticosteroids, immunosuppressants, antibiotics, biologics and surgery. It also discusses managing IBD complications. For IBS, it discusses treatments based on predominant symptoms including fiber, laxatives, antispasmodics, antidiarrheals, 5-HT3/5-HT4 agents and psychotherapy. The document concludes by evaluating