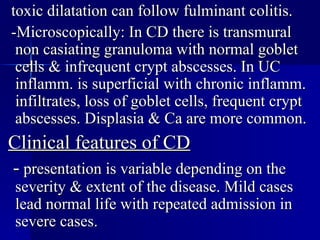
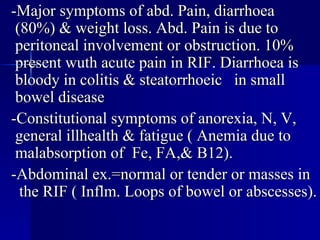
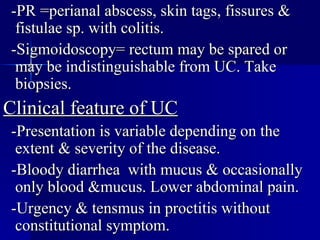
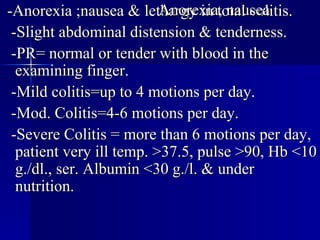
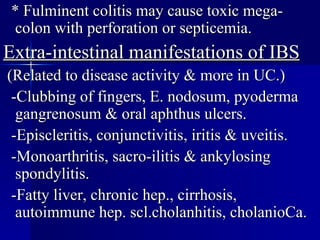
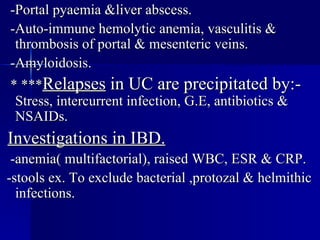
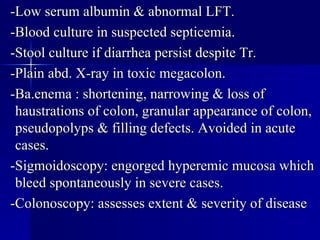
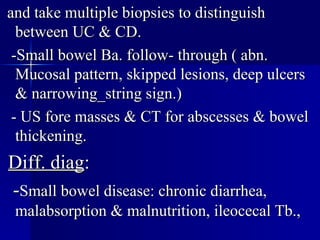
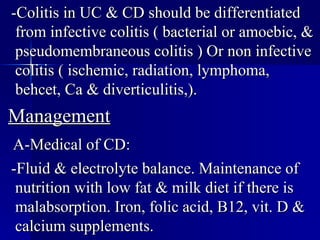
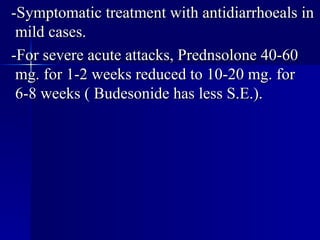
Inflammatory bowel disease (IBD) includes ulcerative colitis and Crohn's disease. IBD is common in Western countries and peaks between ages 20-40, affecting men and women equally. IBD involves periods of remission and relapse. The etiology involves genetic and environmental factors. Diagnosis involves blood tests, stool cultures, imaging tests like CT scans and endoscopy to assess severity and distinguish between UC and CD. Treatment includes medications, diet, surgery, and management of complications.