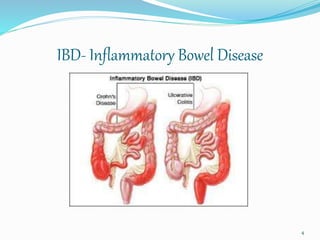
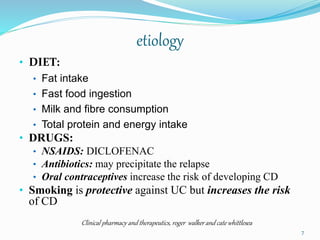
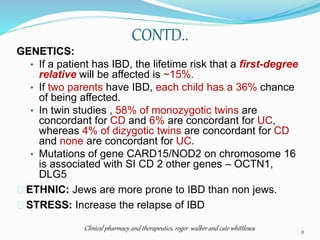
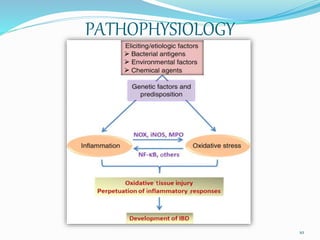
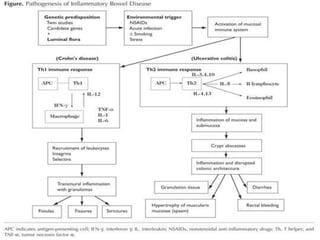
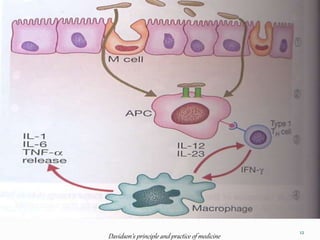
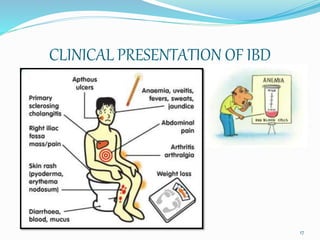
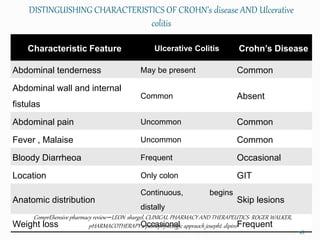
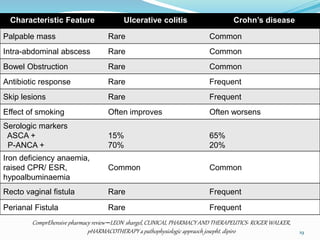
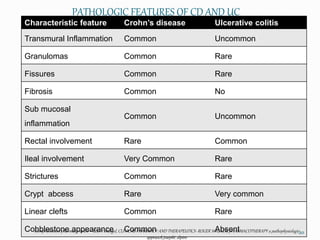
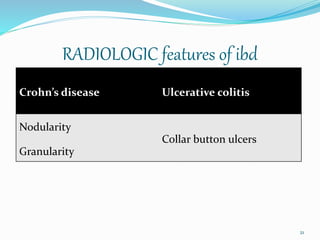
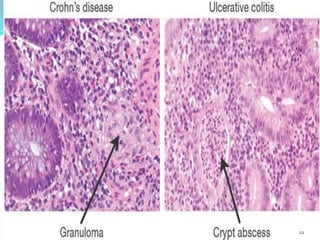
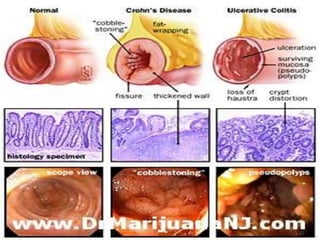
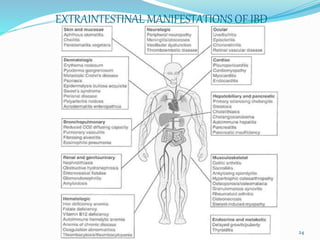
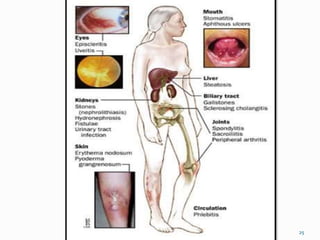
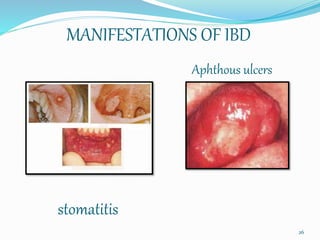
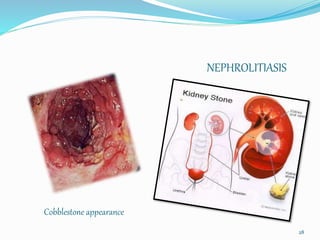
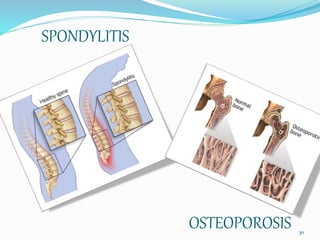
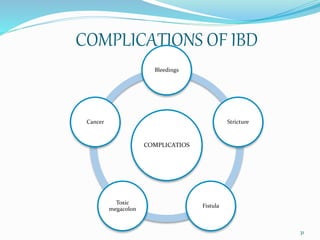
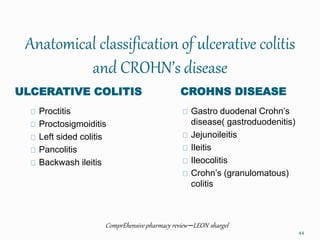
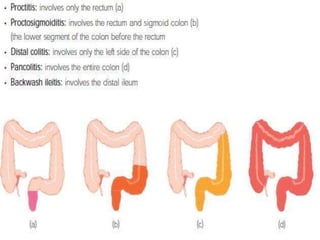
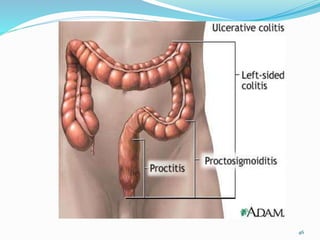
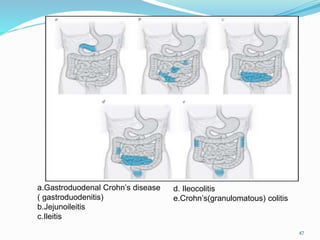
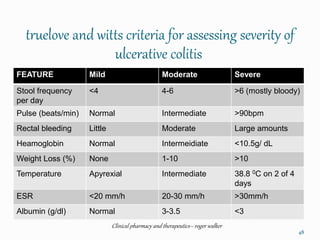
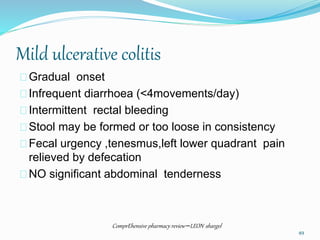
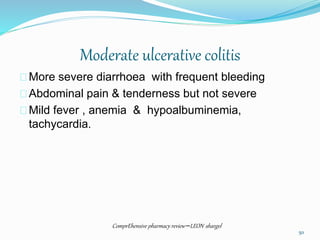
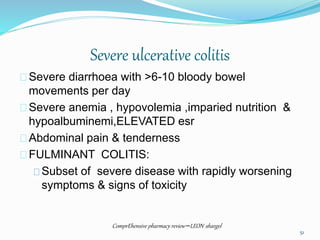
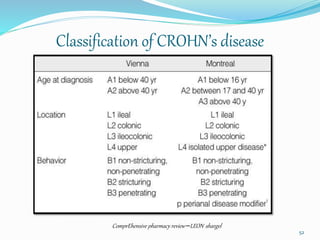
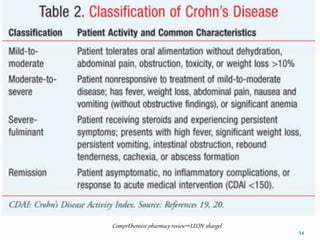
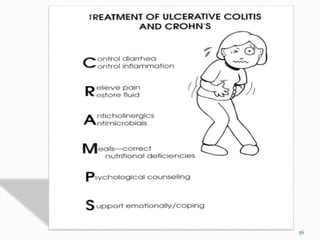
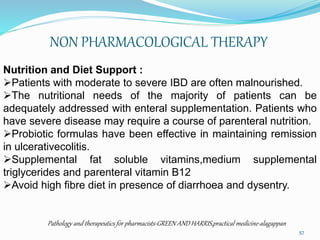
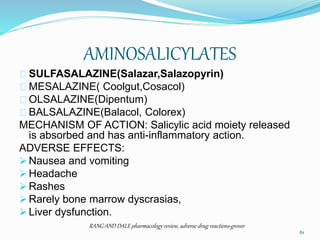
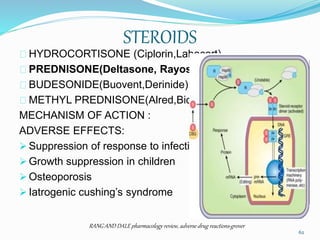
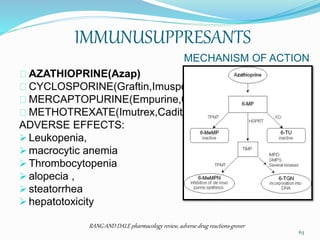
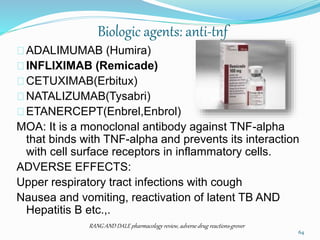
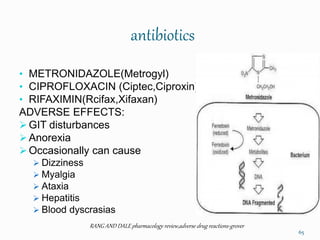
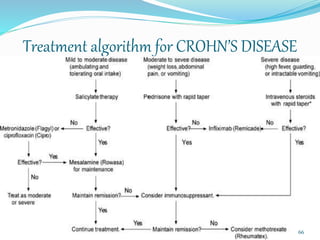
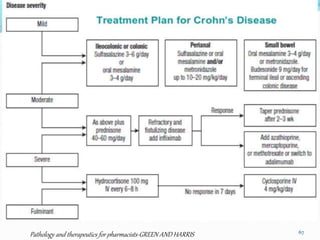
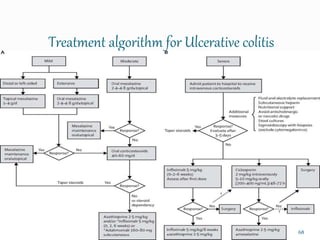
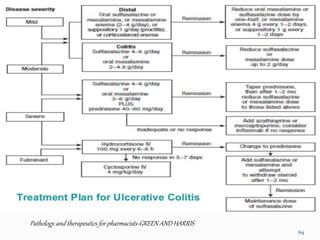
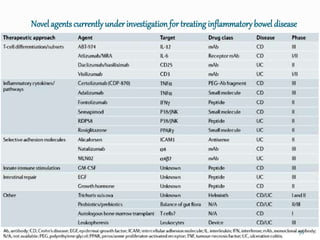
Inflammatory bowel disease (IBD) refers to ulcerative colitis and Crohn's disease, which are chronic inflammatory conditions of the gastrointestinal tract. Ulcerative colitis causes inflammation of the colon, while Crohn's disease causes transmural inflammation that can involve any part of the gastrointestinal tract from mouth to anus. The causes of IBD are not fully understood but involve genetic susceptibility, environmental factors, and dysregulation of the immune system. Symptoms vary depending on the location and severity of inflammation. Treatment involves medications to induce and maintain remission such as aminosalicylates, corticosteroids, immunomodulators, antibiotics, biologics, and surgery for complications.