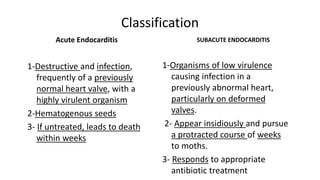
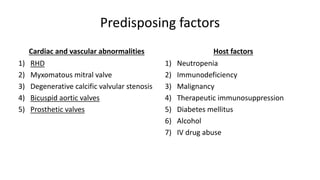
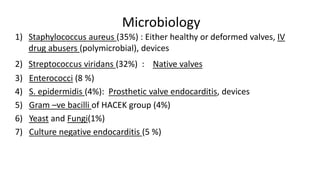
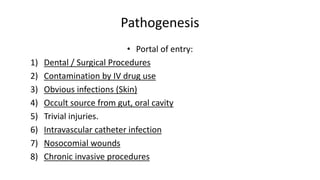
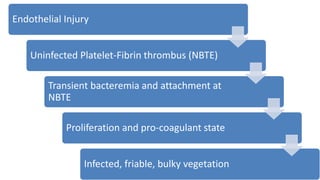
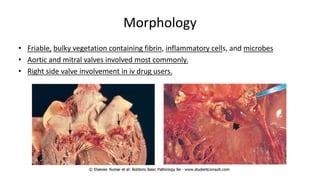
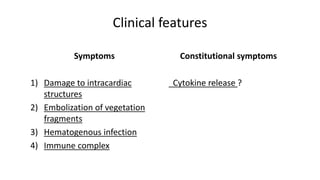
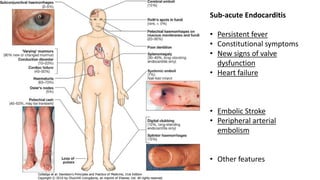
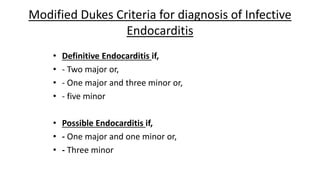
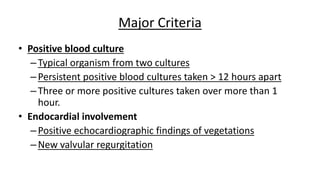
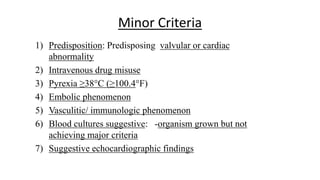
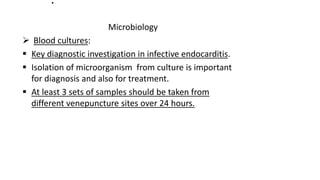
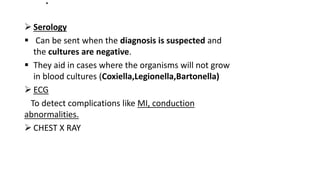
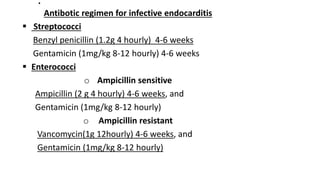
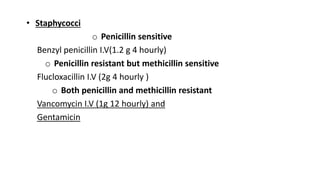
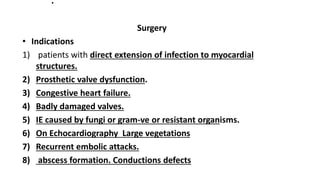
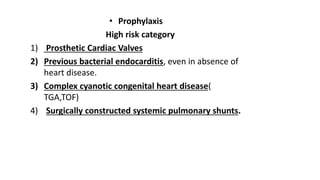
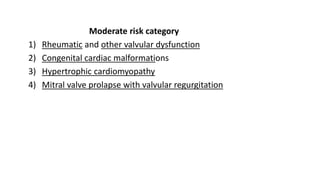
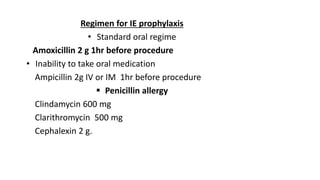
Infective Endocarditis is an infection of the heart valves or endocardium. It is characterized by vegetation formation on the valves due to bacterial colonization. It can affect native or prosthetic valves. There are different classifications based on the virulence of the organism and severity. Predisposing factors include underlying heart conditions and immunosuppression. Common causative organisms are staphylococci and streptococci. Diagnosis is based on modified Dukes criteria using blood cultures, echocardiography and clinical features. Treatment involves long-term antibiotic therapy based on the identified organism along with surgery in some severe cases. Endocarditis prophylaxis is recommended for high risk patients undergoing certain medical procedures.