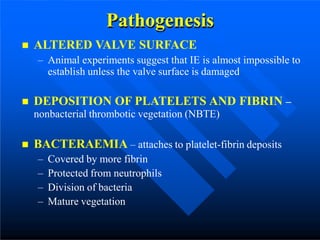
Infective endocarditis is a microbial infection of the heart valves or endocardium. It is characterized by pathological vegetations composed of platelets, fibrin, microorganisms, and inflammatory cells. It occurs more commonly in males and the elderly. It can be acute, affecting normal valves rapidly, or subacute, often affecting damaged valves in a slower manner. Bacteria enter the bloodstream and attach to platelet-fibrin deposits on damaged heart valves. Diagnosis involves blood cultures, echocardiography, and applying the Duke criteria. Complications include embolisms, local or metastatic infection spread, and immune complex disease. Treatment involves antibiotics, sometimes with surgery. High-risk patients may receive antibiotic prophylaxis