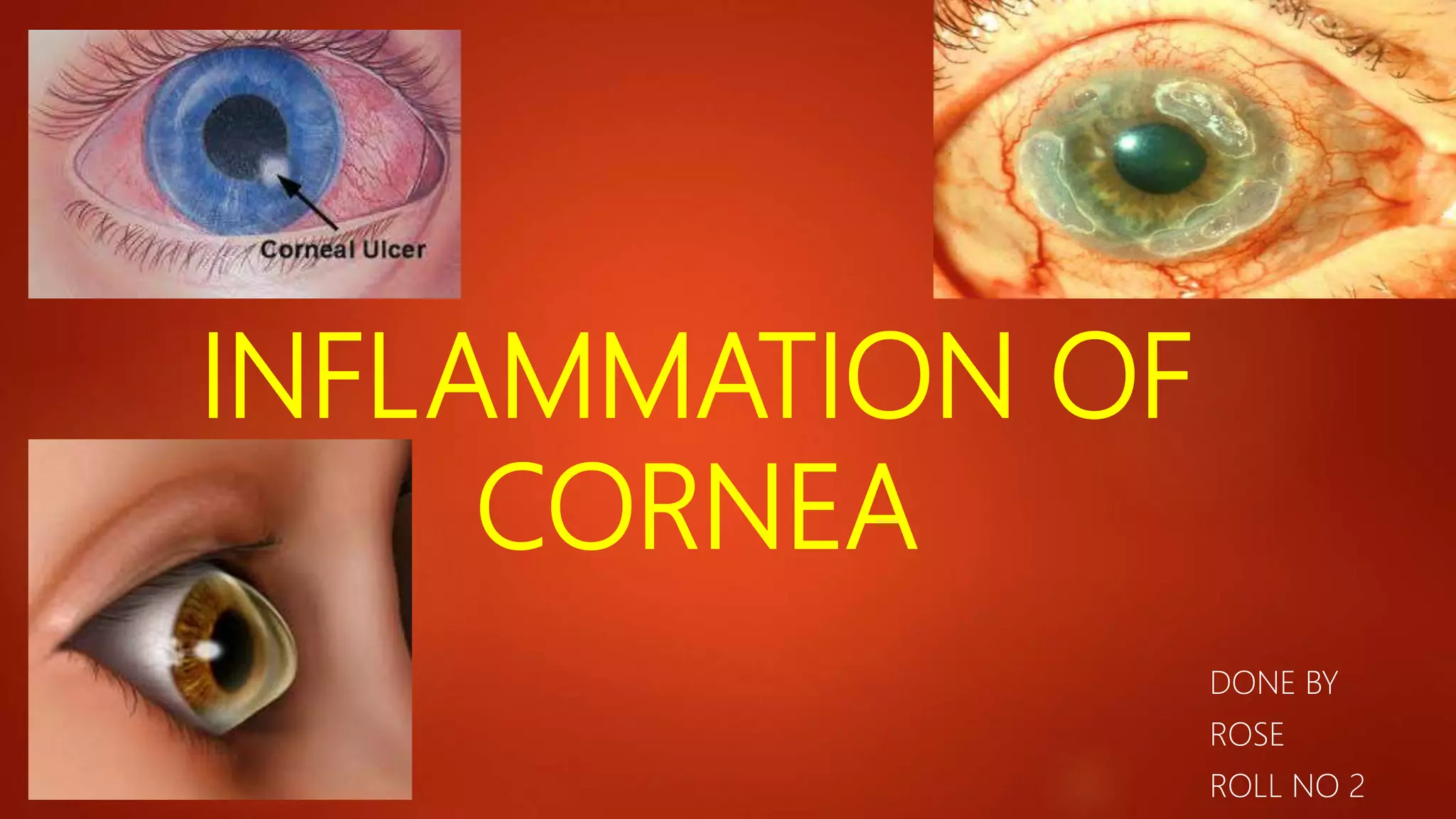
This document describes different types of keratitis, including ulcerative keratitis, non-ulcerative keratitis, and infective keratitis caused by bacteria, fungi, viruses, and protozoa. It discusses the classification, etiology, signs, diagnosis, and management of various forms of corneal inflammation and infection. Key pathogens mentioned include Staphylococcus aureus, Pseudomonas, herpes simplex virus, acanthamoeba, and fungi like Aspergillus and Fusarium.