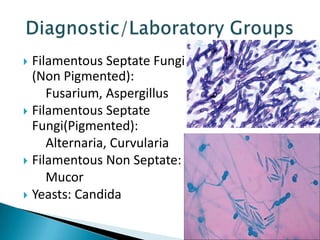
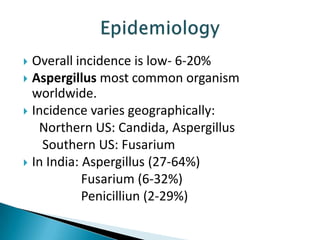
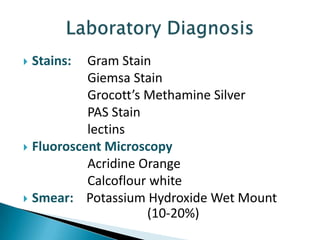
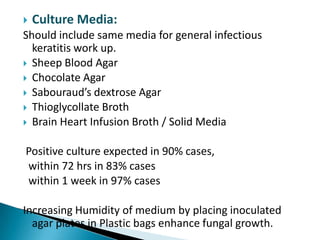
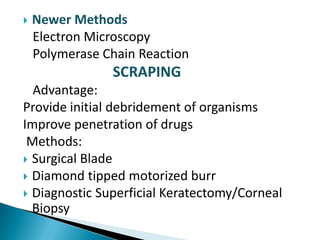
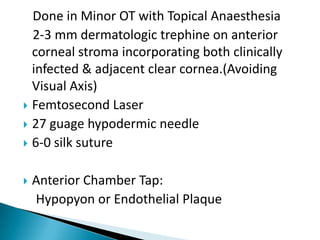
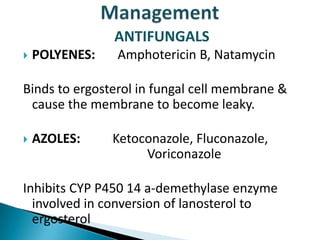
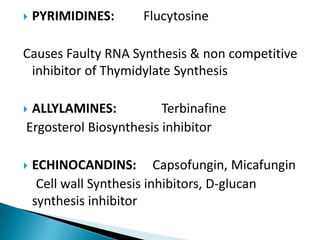
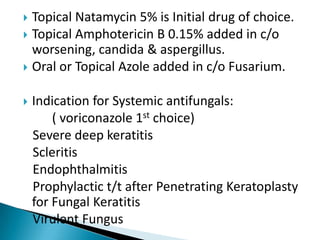
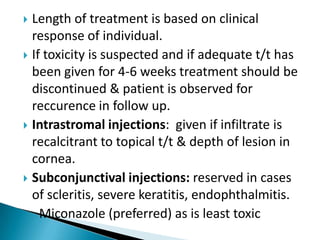
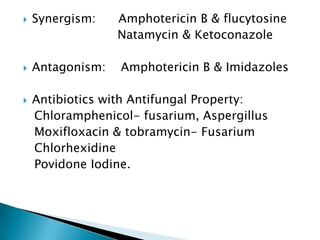
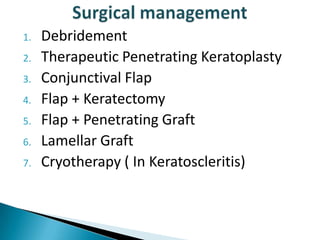
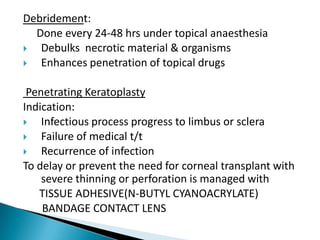
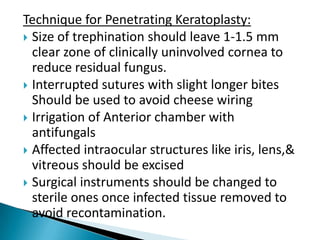
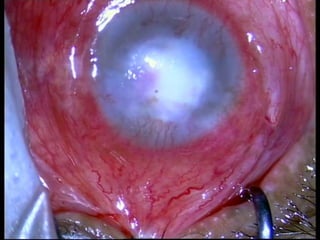
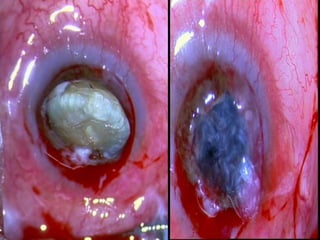
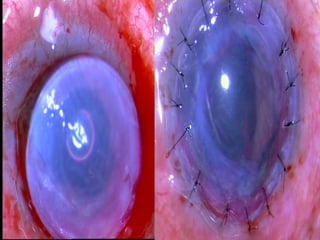
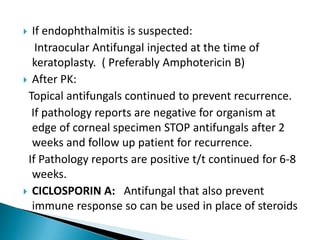
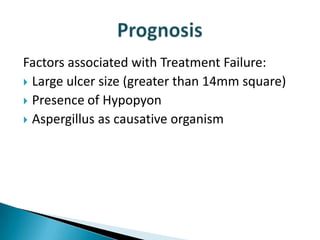
Fungal keratitis is difficult to diagnose and treat. Common causative fungi include Aspergillus, Candida, and Fusarium. Diagnosis involves potassium hydroxide wet mount, stains like Gram or Grocott's, and culture. Topical natamycin is first-line treatment but systemic antifungals like voriconazole may be needed for severe cases. Management also includes frequent debridement and potentially therapeutic penetrating keratoplasty for non-responsive or advanced cases. Prognosis depends on factors like ulcer size and presence of hypopyon.