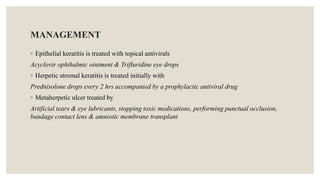
The document outlines infective corneal ulcers, detailing their definitions, types, etiologies, symptoms, diagnosis, and management principles. It emphasizes the distinction between infectious and non-infectious keratitis, highlighting the critical need for timely treatment to prevent vision loss. The management strategies include infection control, inflammation management, and re-epithelialization promotion, with specific treatments based on the underlying cause of the corneal ulcer.