This document provides information on classifying primary bone tumors based on location and radiographic appearance. Key points include:
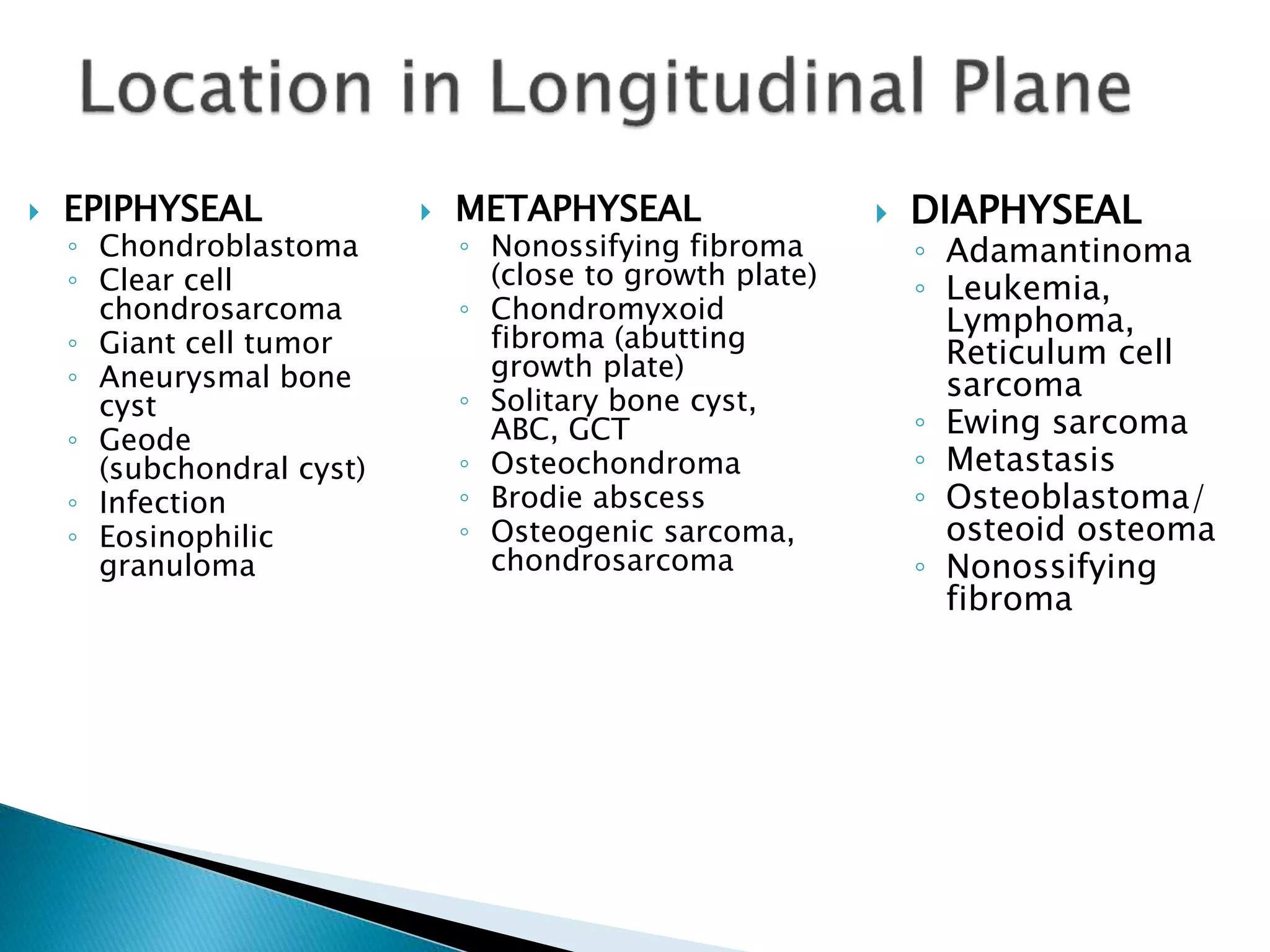
- Location within the bone (epiphyseal, diaphyseal, metaphyseal) and age of the patient help classify tumors.
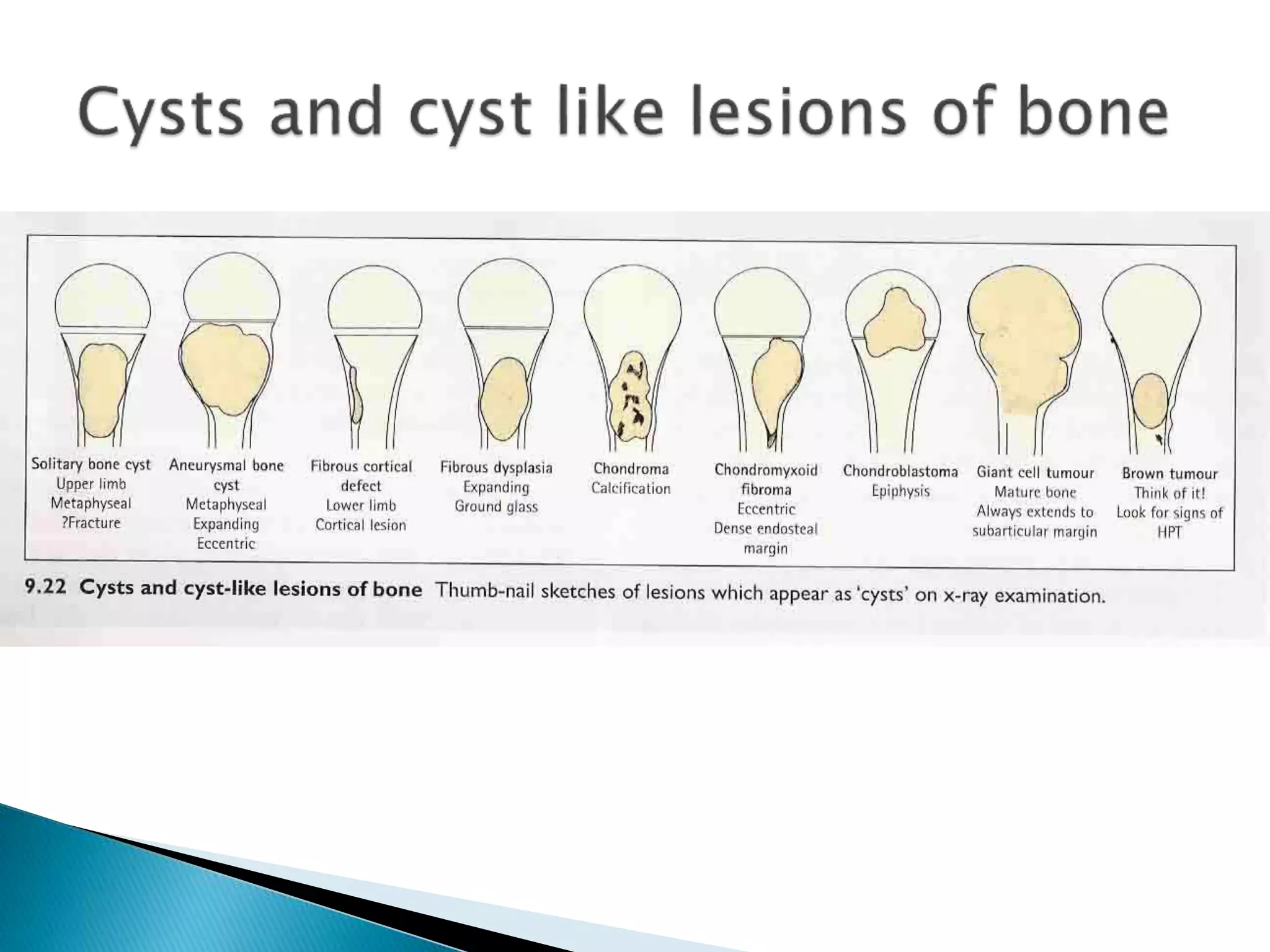
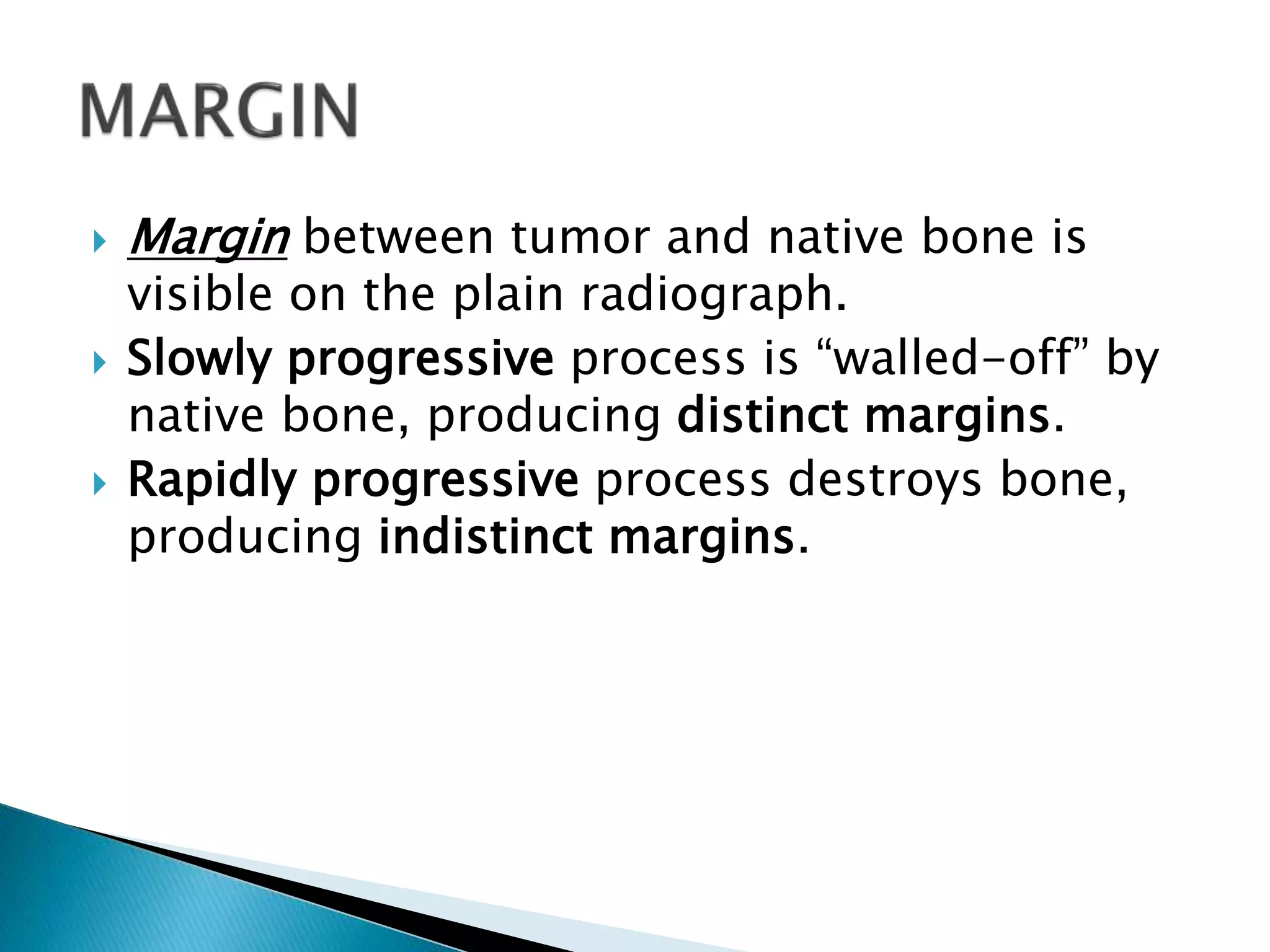
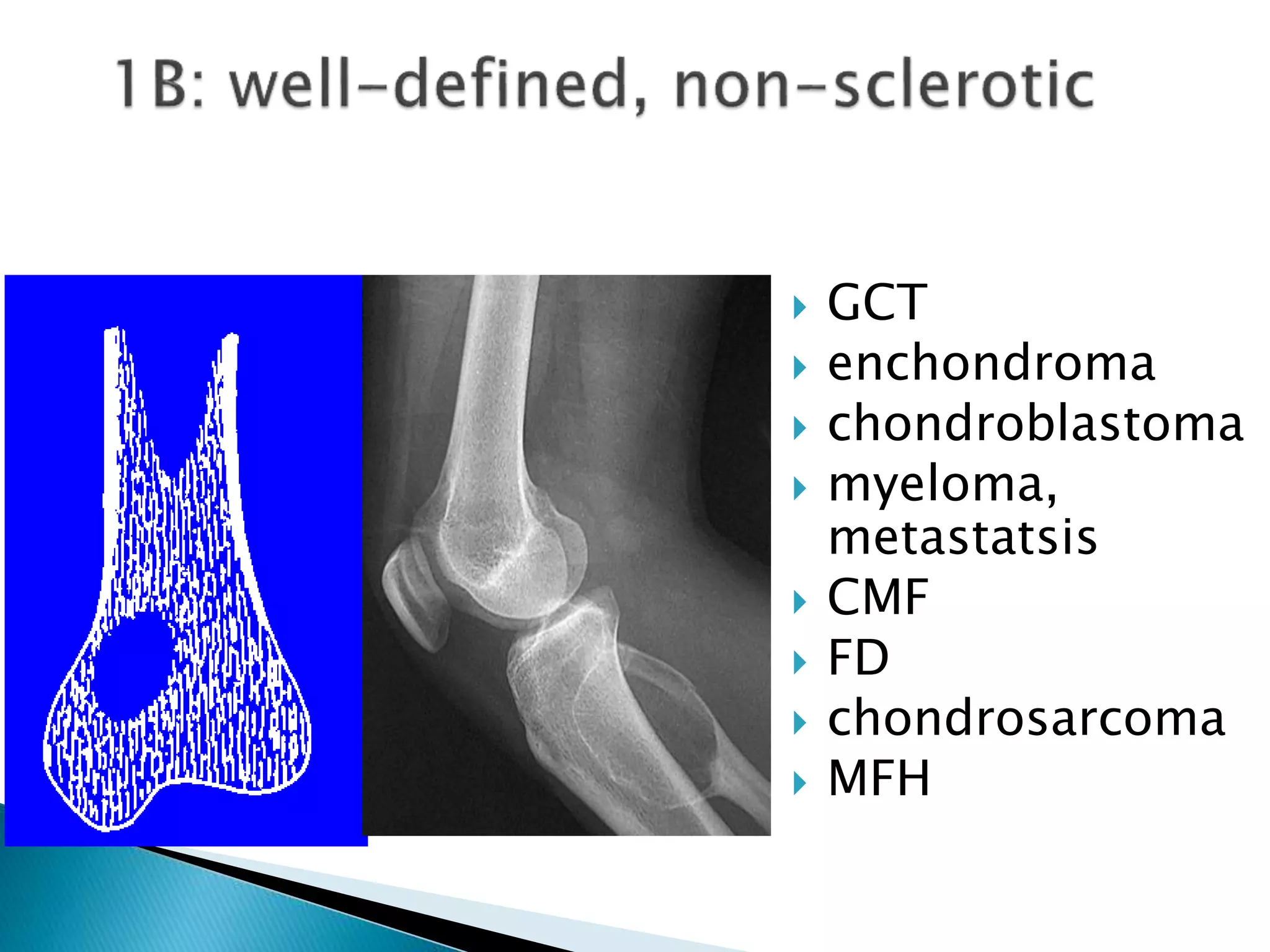
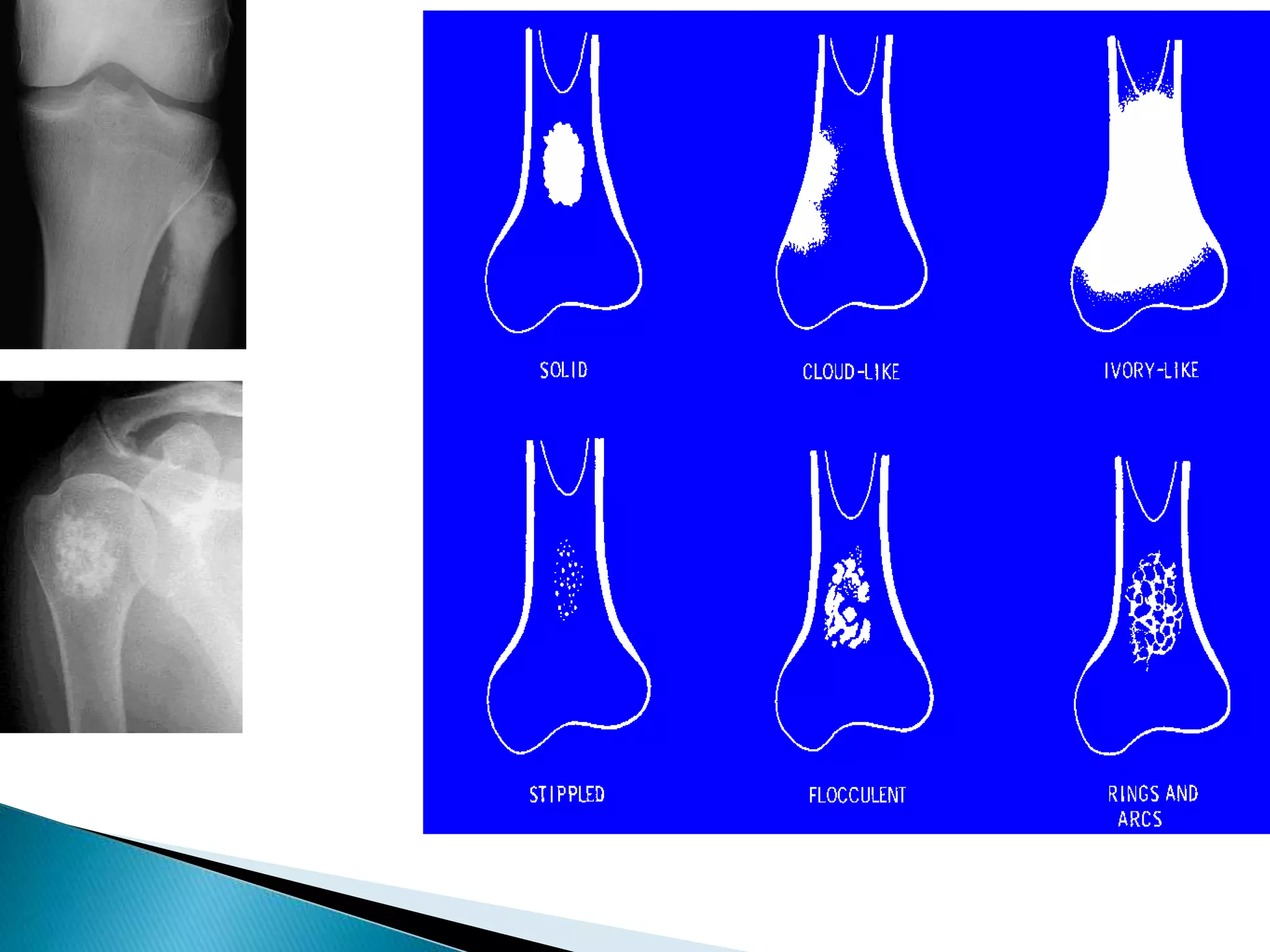
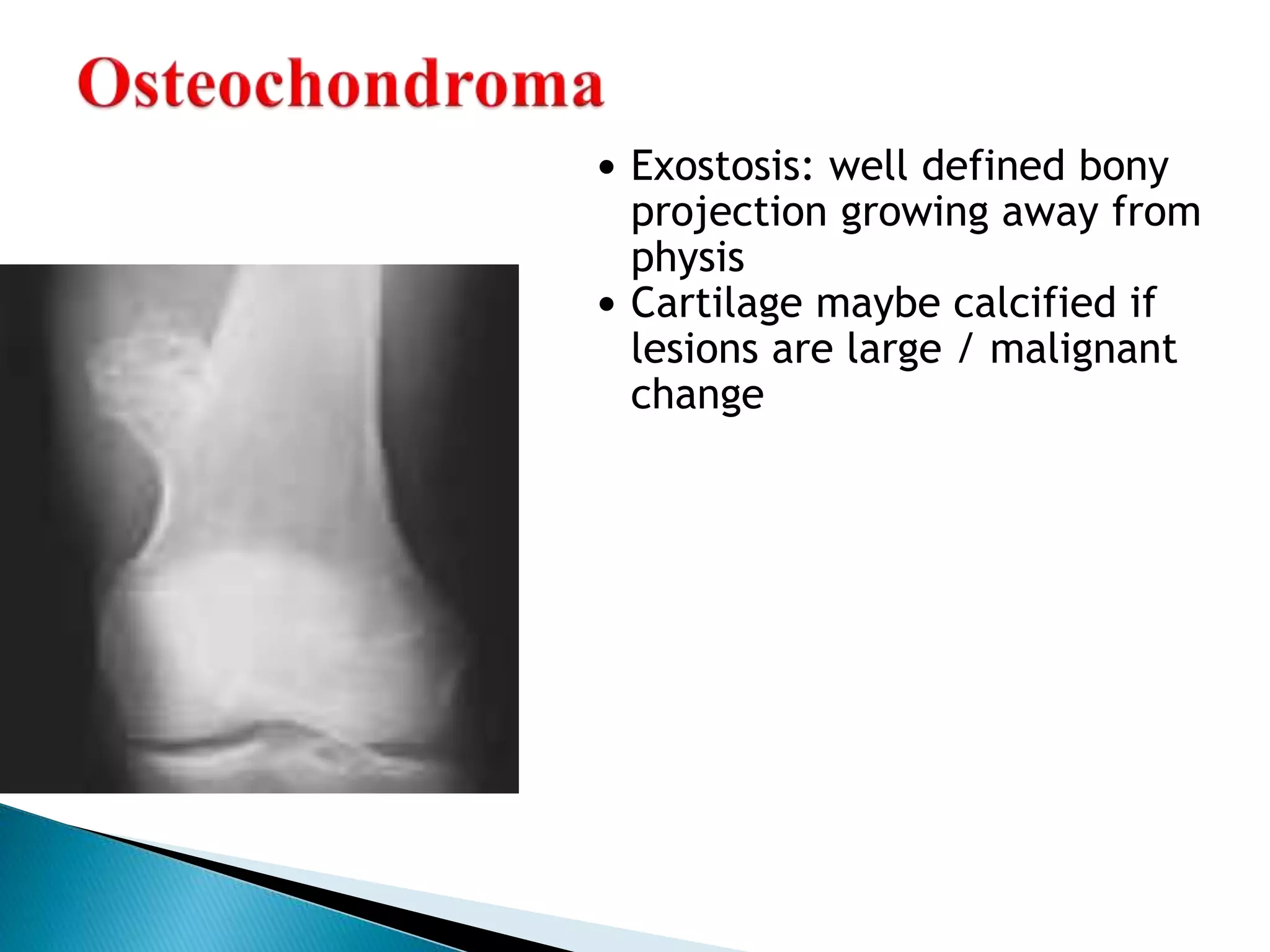
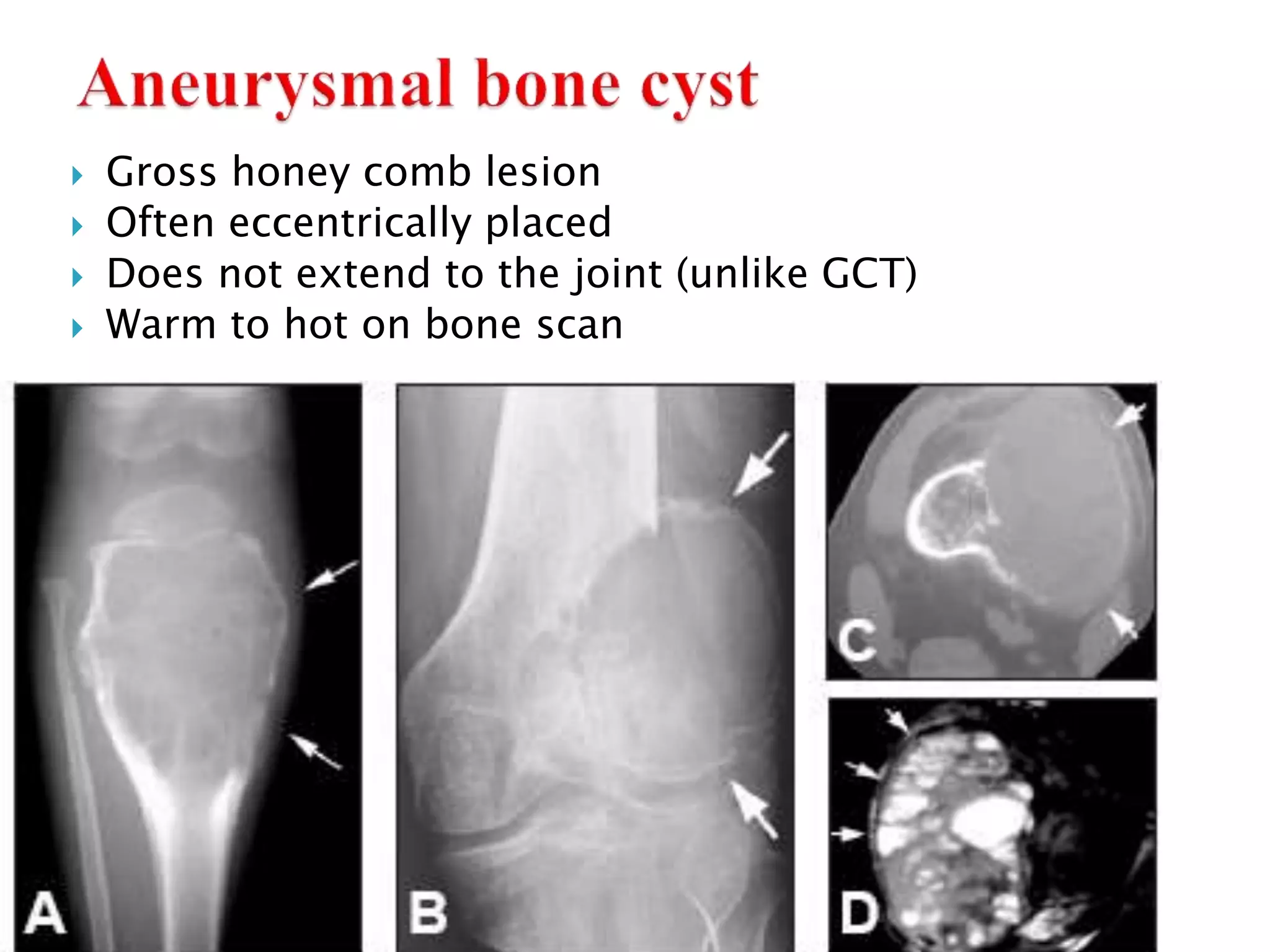
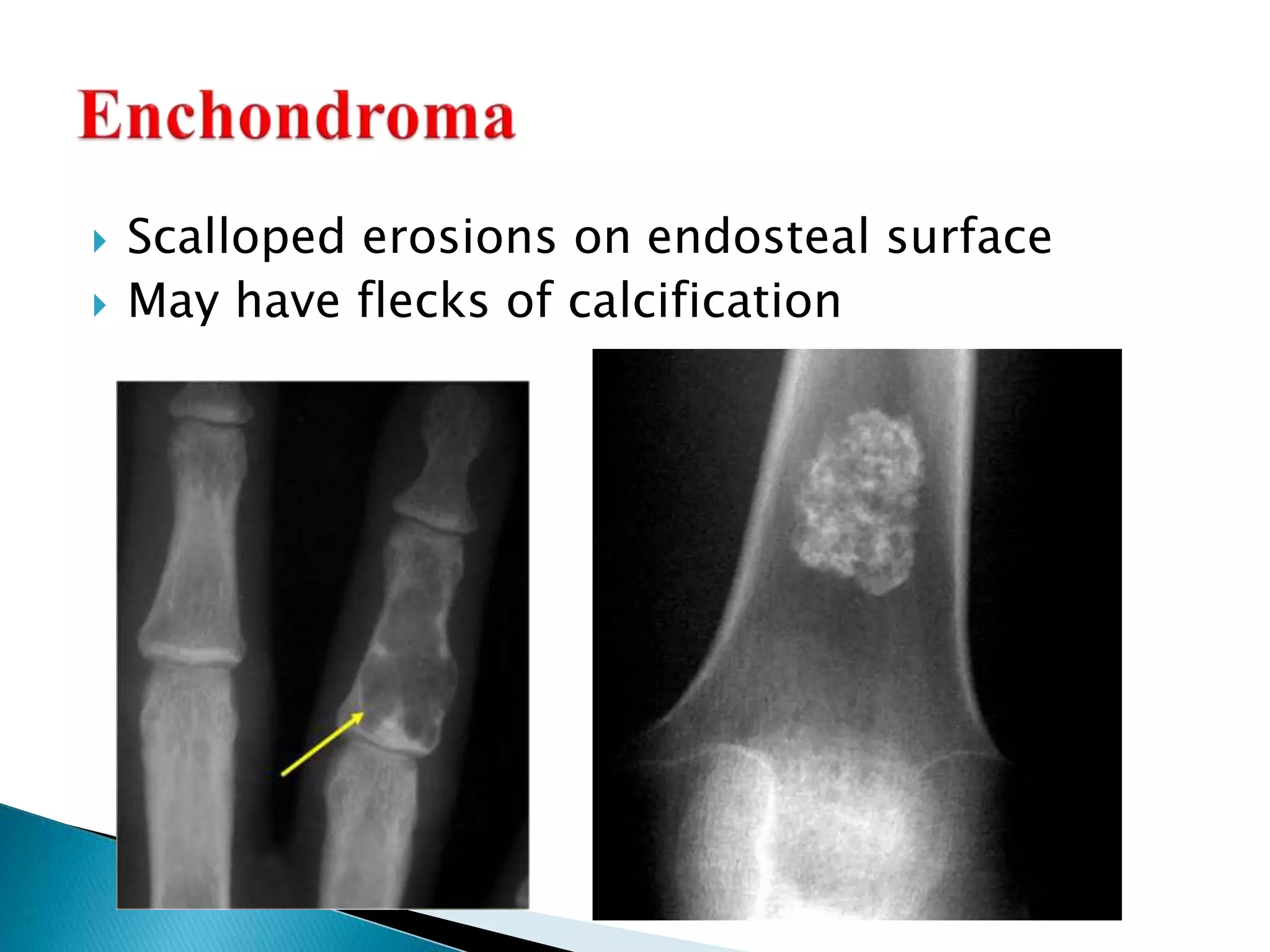
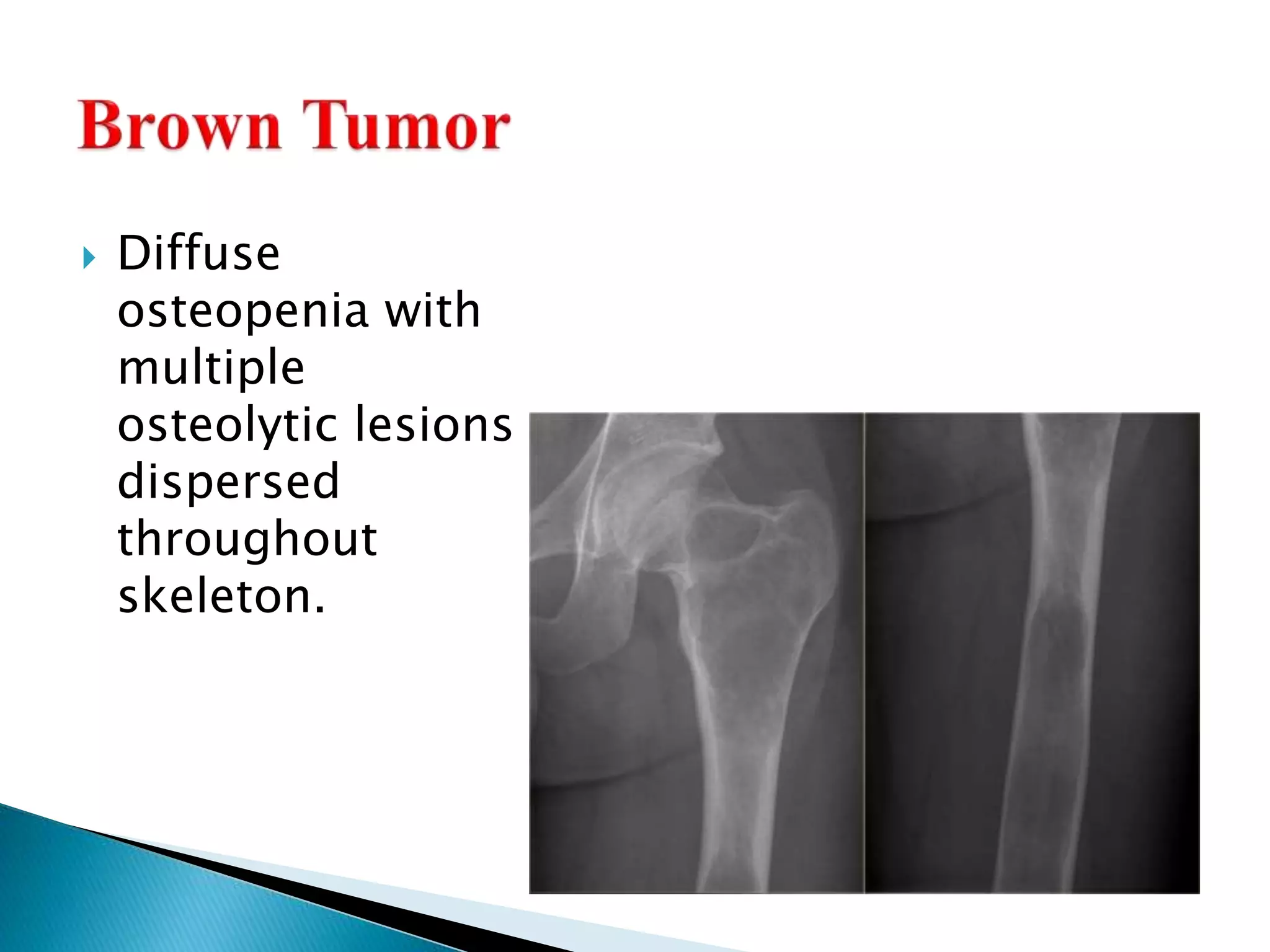
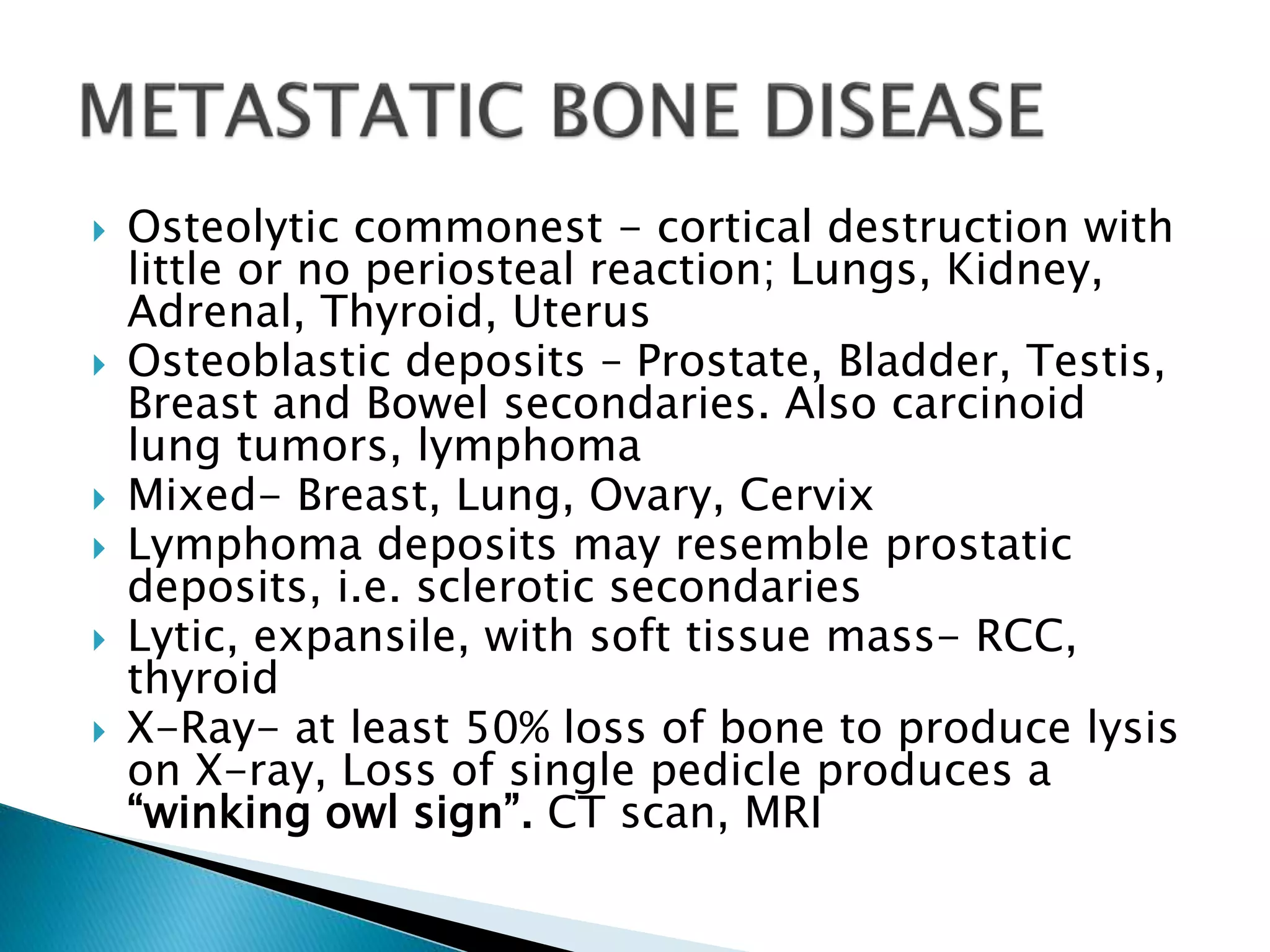
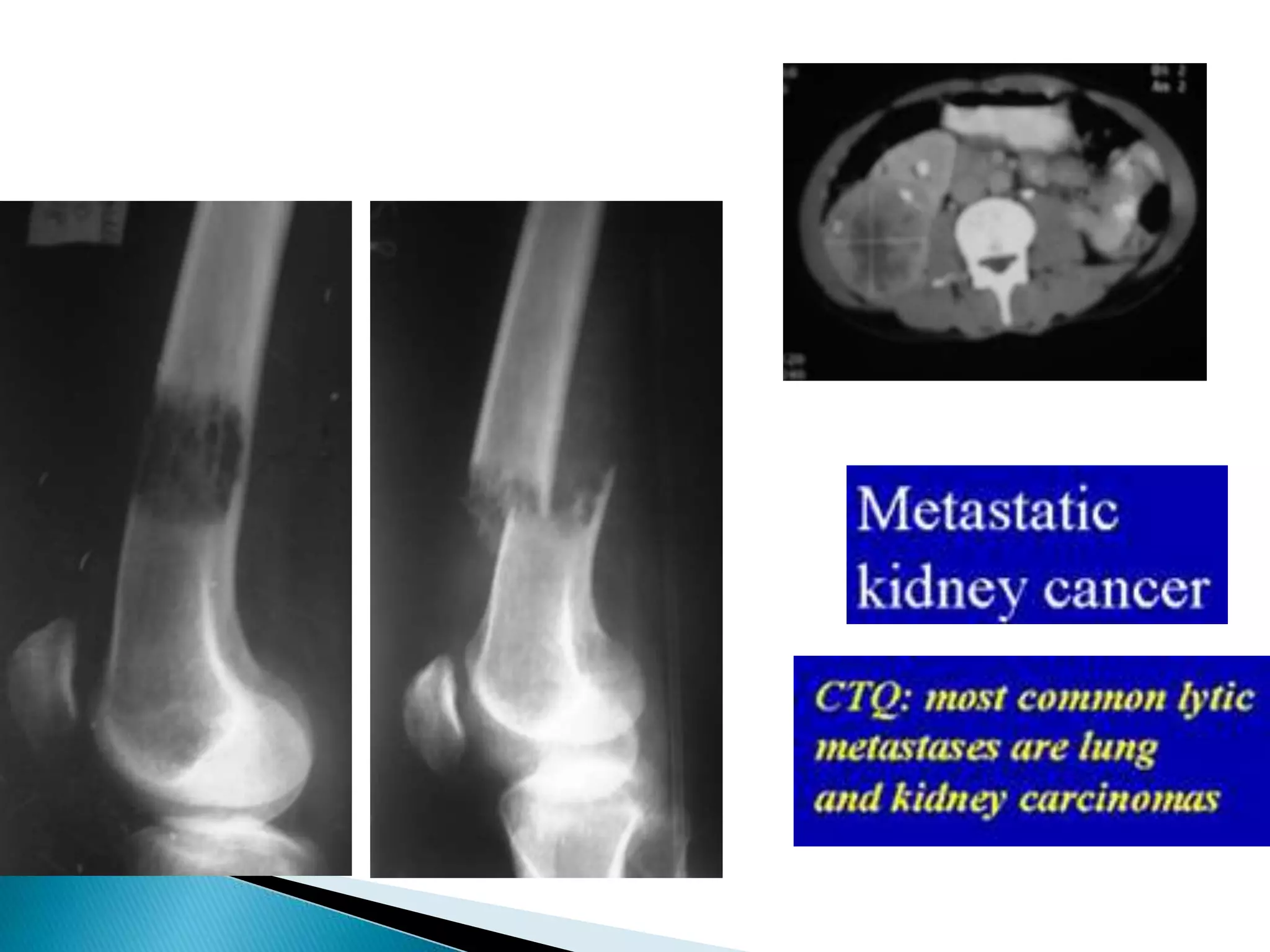
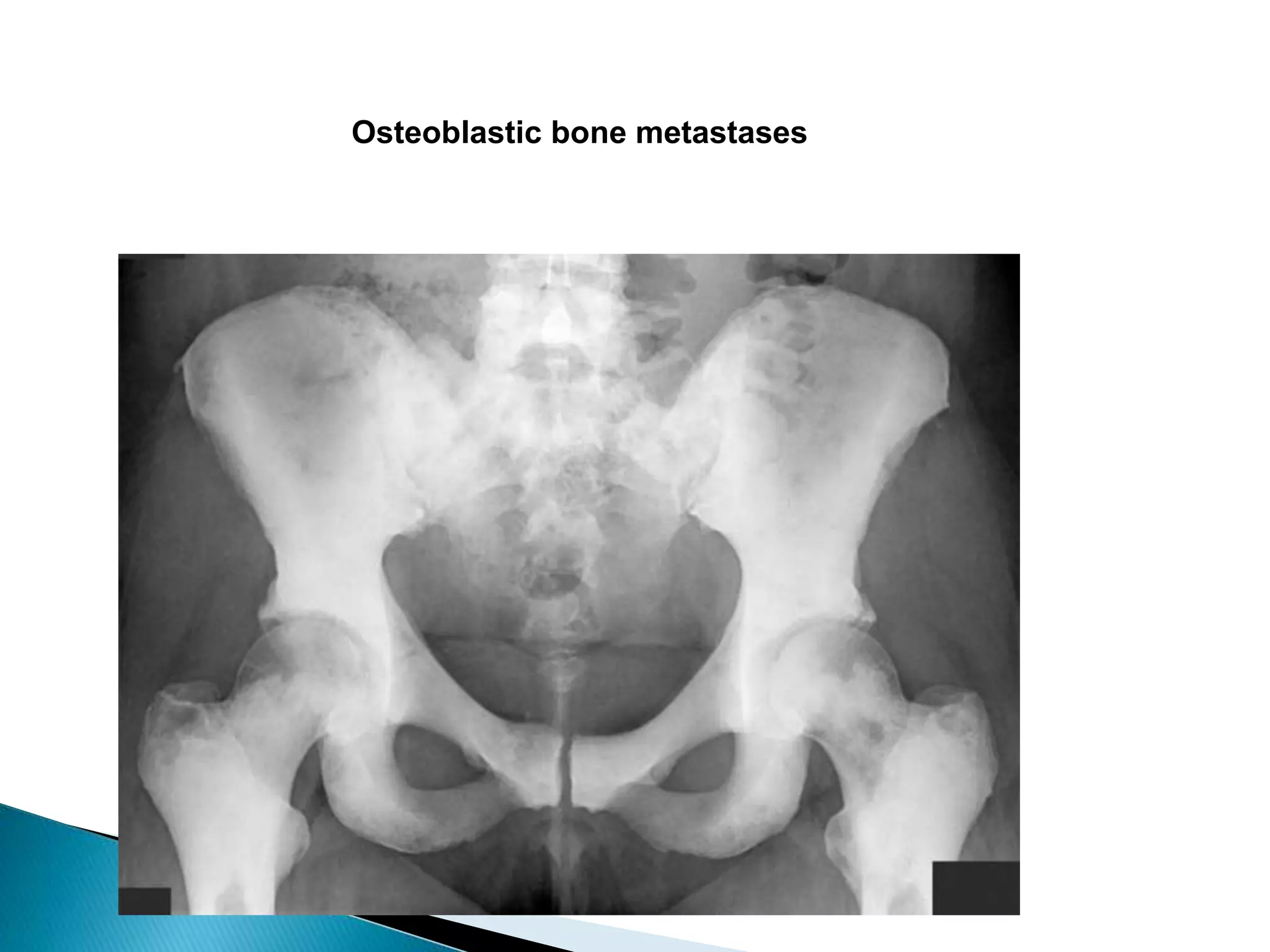
- Features like margins, extent of bone destruction/formation, and presence of a matrix provide clues about tissue type and aggressiveness.
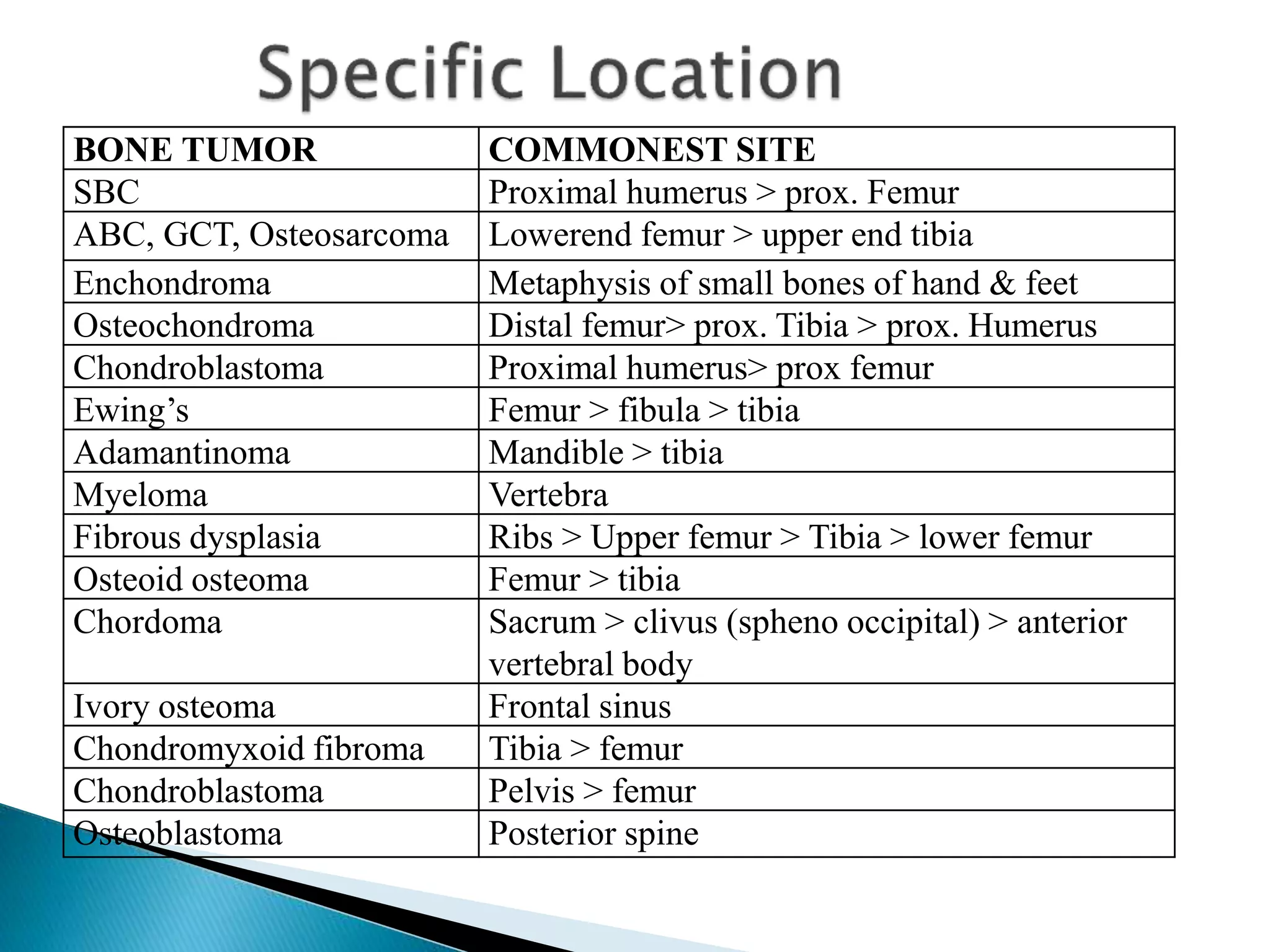
- Common sites for different tumors are listed to aid diagnosis.
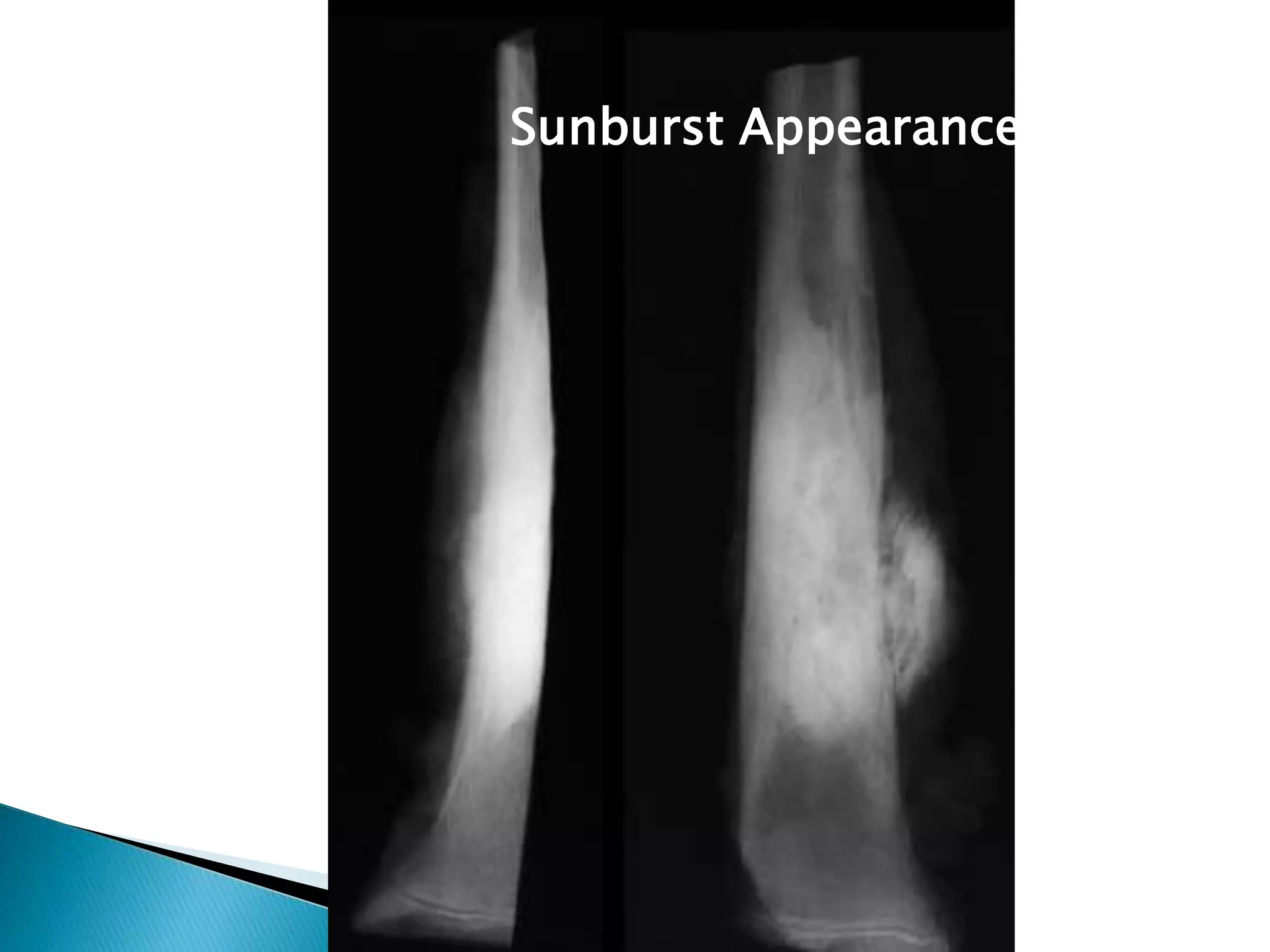
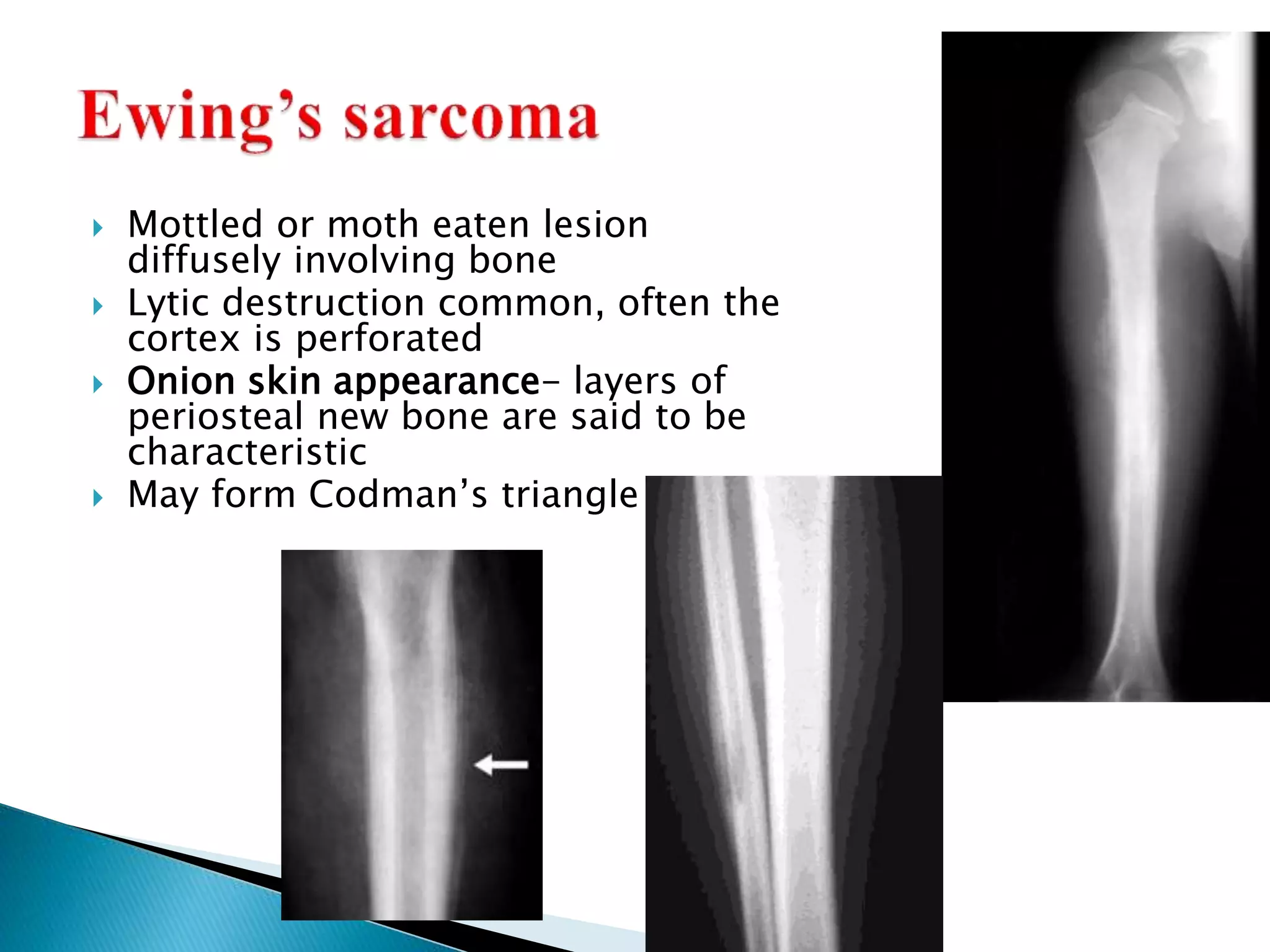
- Patterns of bone destruction (lytic, motheaten) and periosteal reactions further characterize lesions.