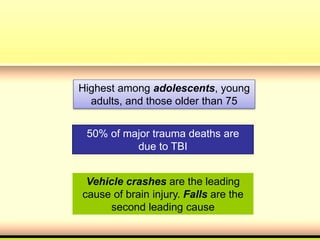
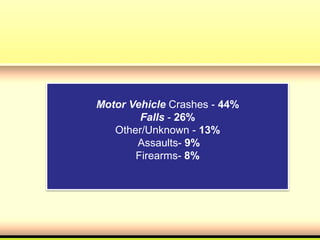
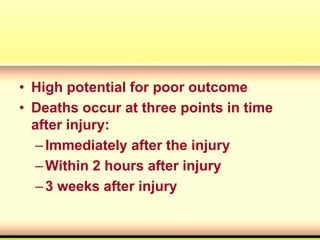
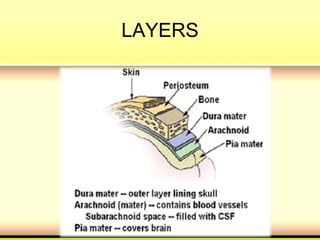
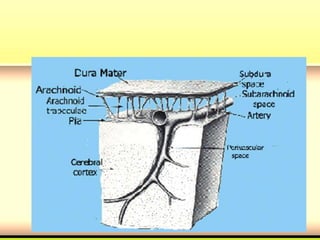
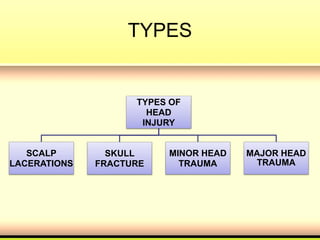
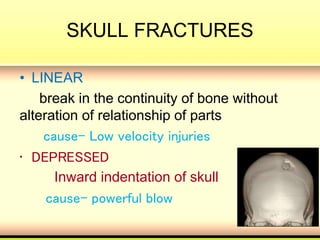
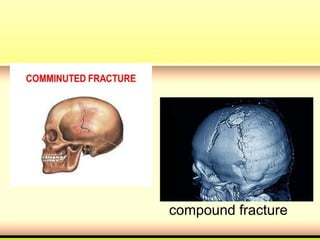
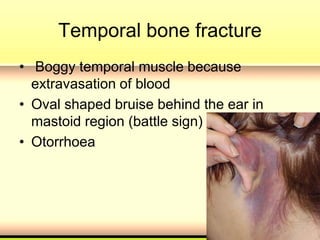
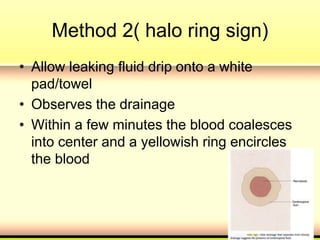
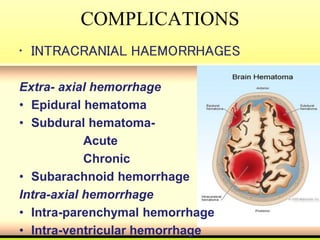
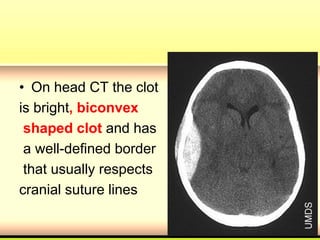
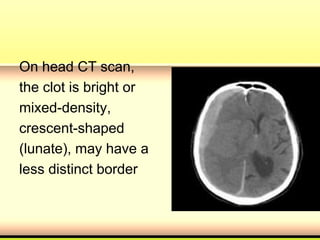
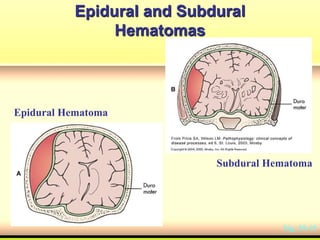
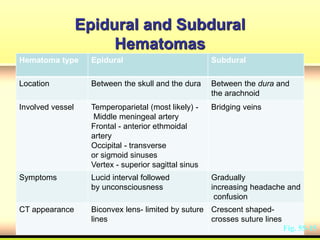
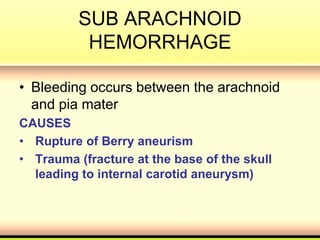
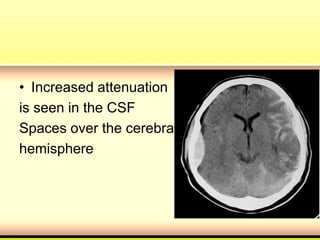
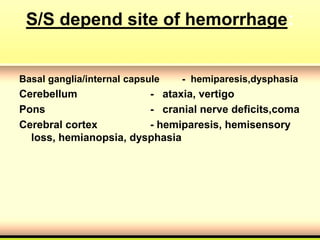
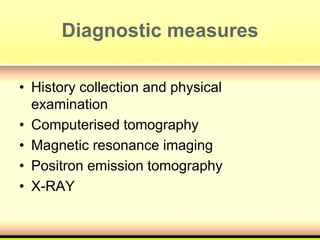
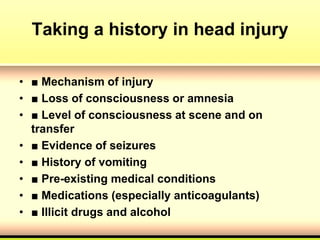
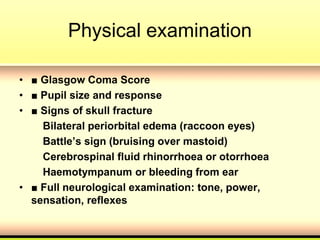
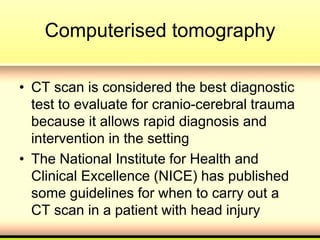
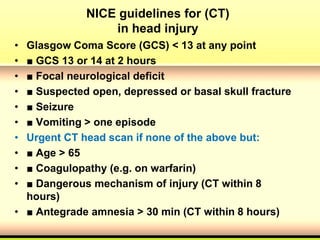
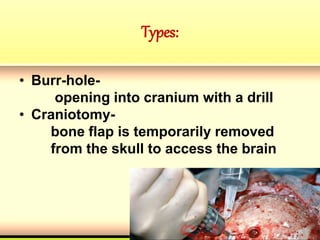
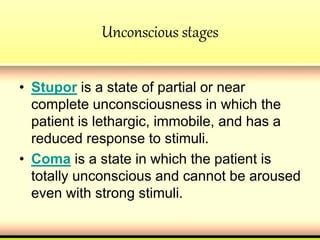
This document provides an overview of the management of head injuries. It defines different types of head injuries from scalp lacerations to traumatic brain injuries. It describes the most common causes of head injuries and explains the layers of the head. It then details different types of head injuries including concussions, skull fractures, and intracranial hemorrhages. It outlines the clinical presentation, diagnostic tools, and management approaches for various head injuries.