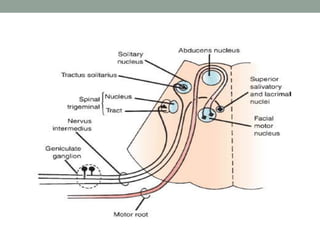
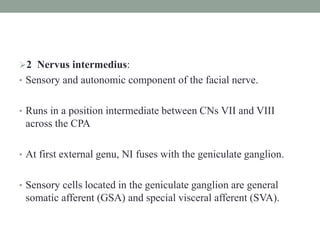
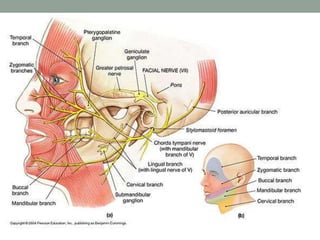
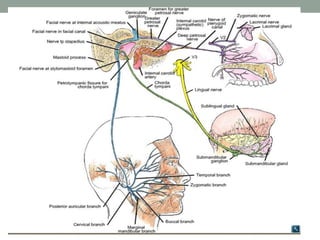
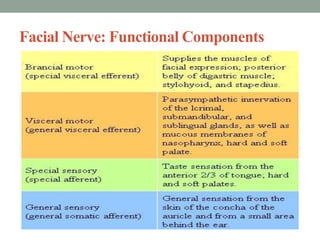
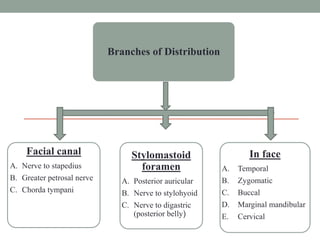
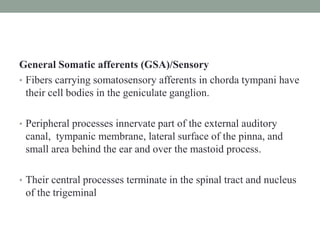
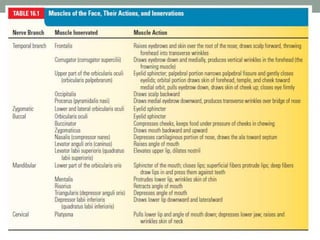
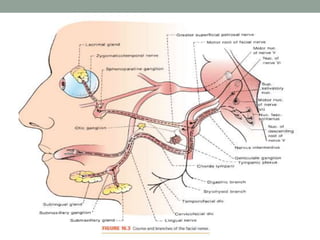
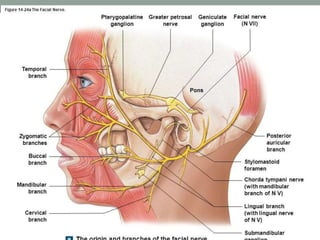
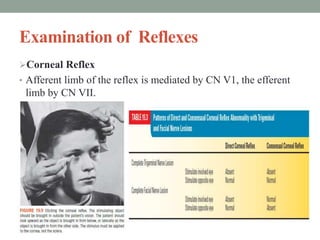
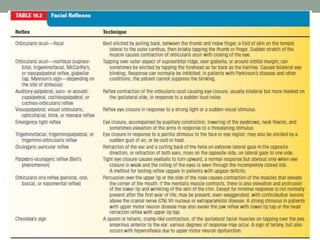
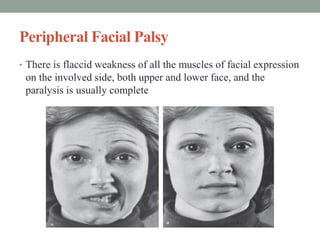
The facial nerve is a mixed nerve that controls muscles of facial expression and sensation. It has motor, sensory, and parasympathetic components. The motor component innervates muscles of the face and head. The sensory component conveys taste from the tongue and sensation from the ear. The parasympathetic component regulates salivary and tear glands. Examination of the facial nerve tests motor function by asking the patient to move facial muscles, sensory function by testing taste and ear sensation, and secretory function by measuring tear and saliva levels.