- Physiological variations in children such as intoeing, out-toeing, bowing of the legs, and flat feet are common and usually resolve on their own without intervention. Conditions that suggest an abnormality include asymmetry, limitation of movement, or progressive deformity.
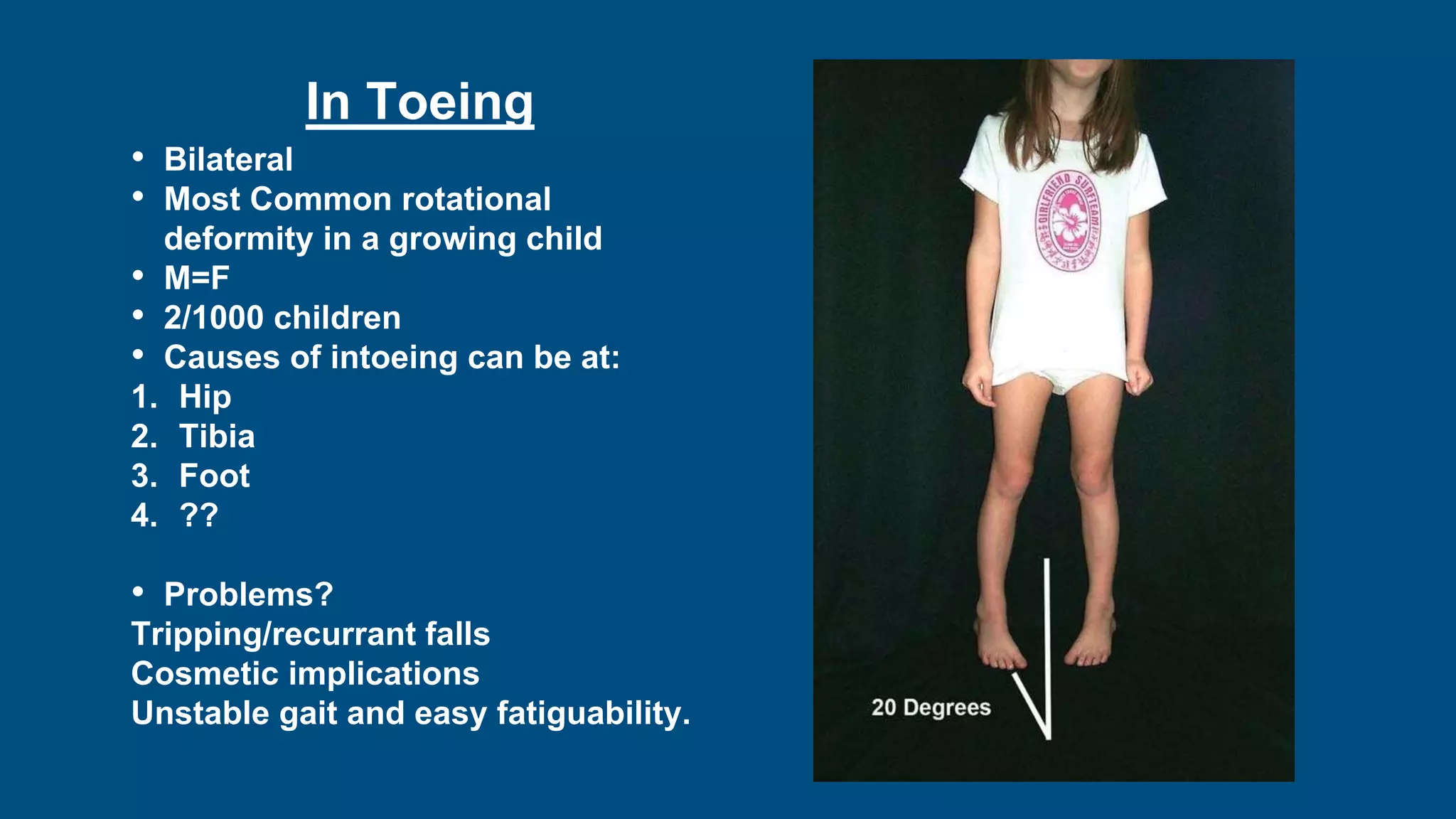
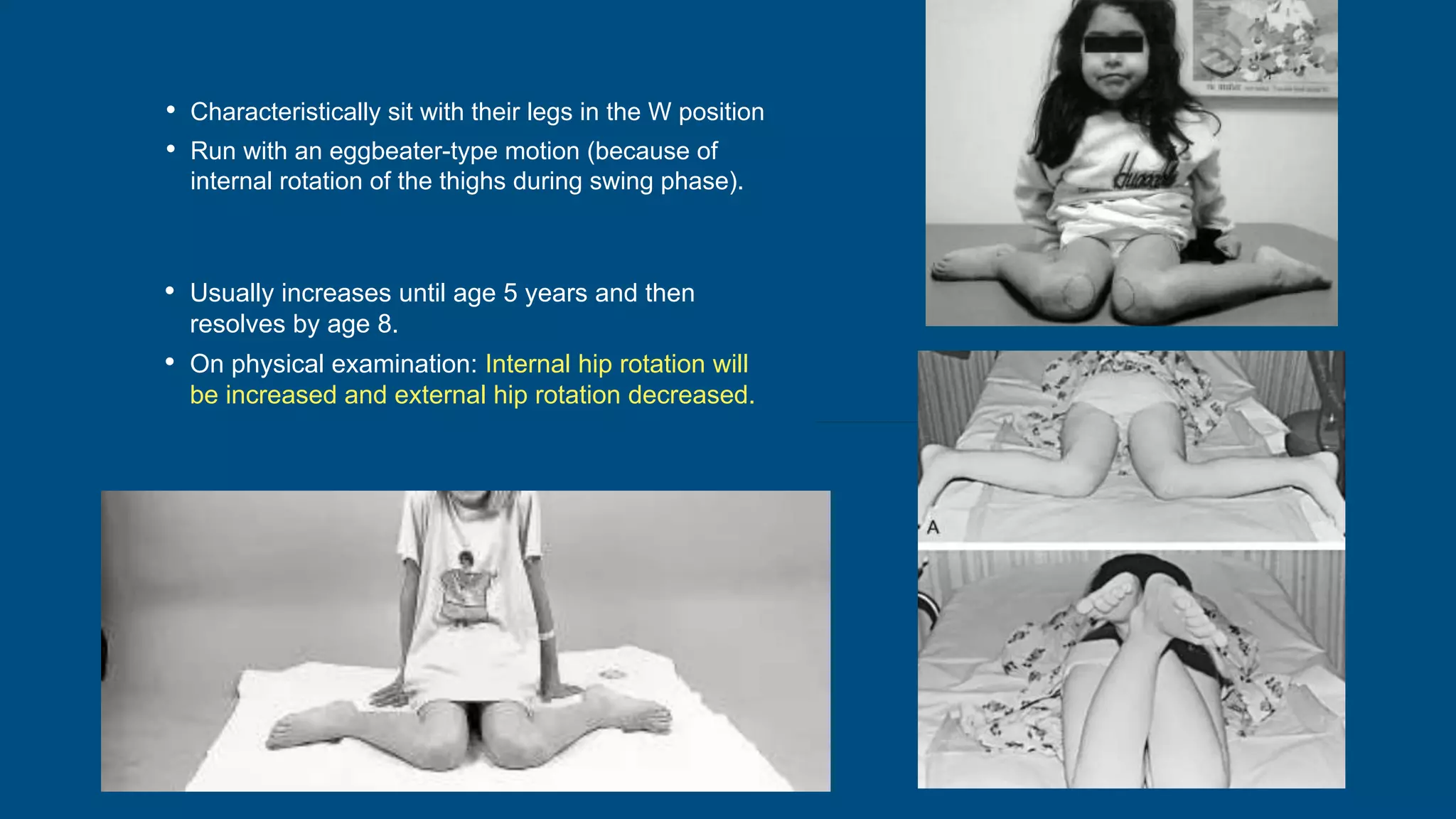
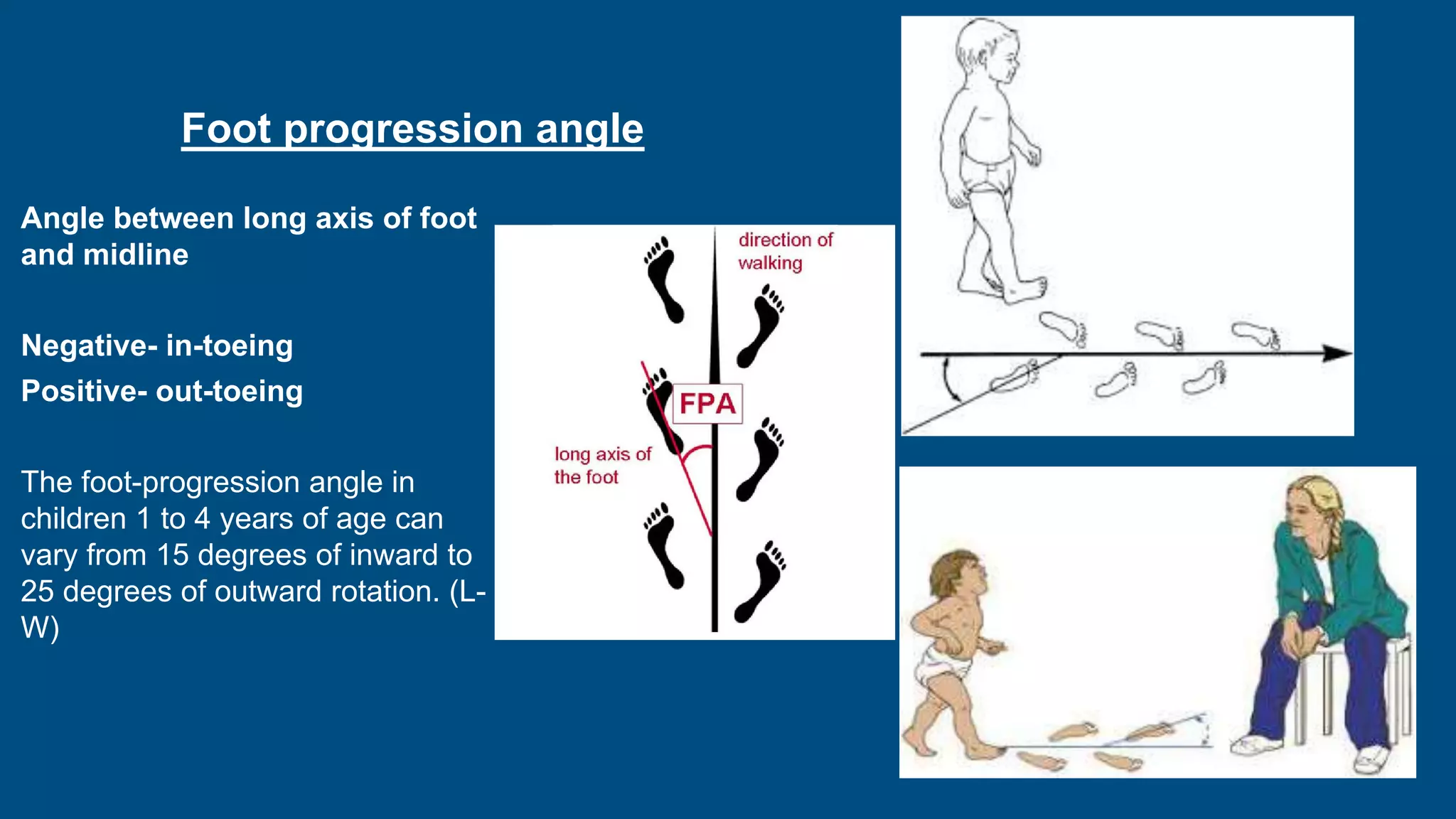
- Intoeing is most commonly caused by femoral anteversion or tibial torsion in young children and resolves by age 8 in 95% of cases. Out-toeing can be due to femoral retroversion or external tibial torsion.
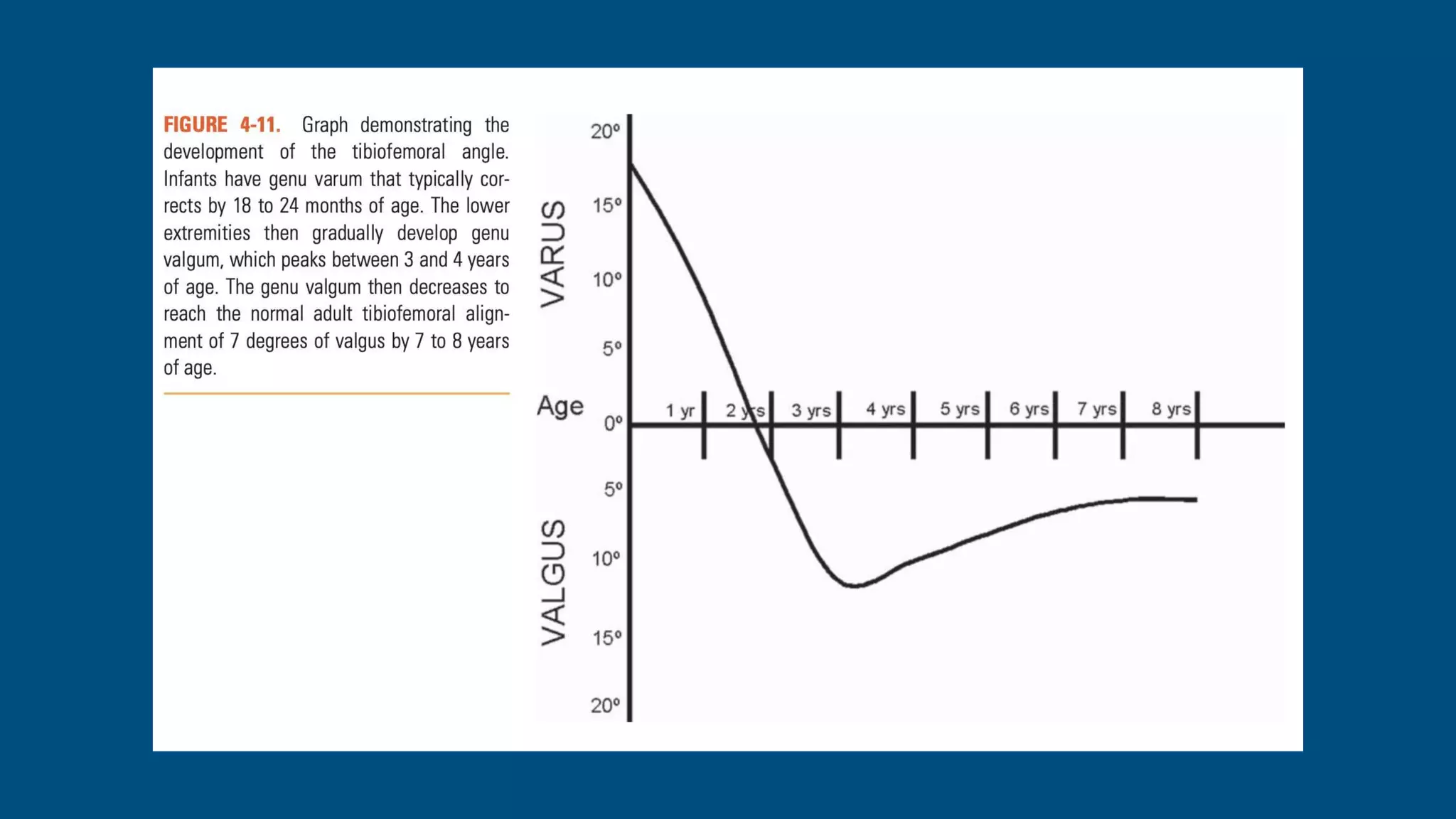
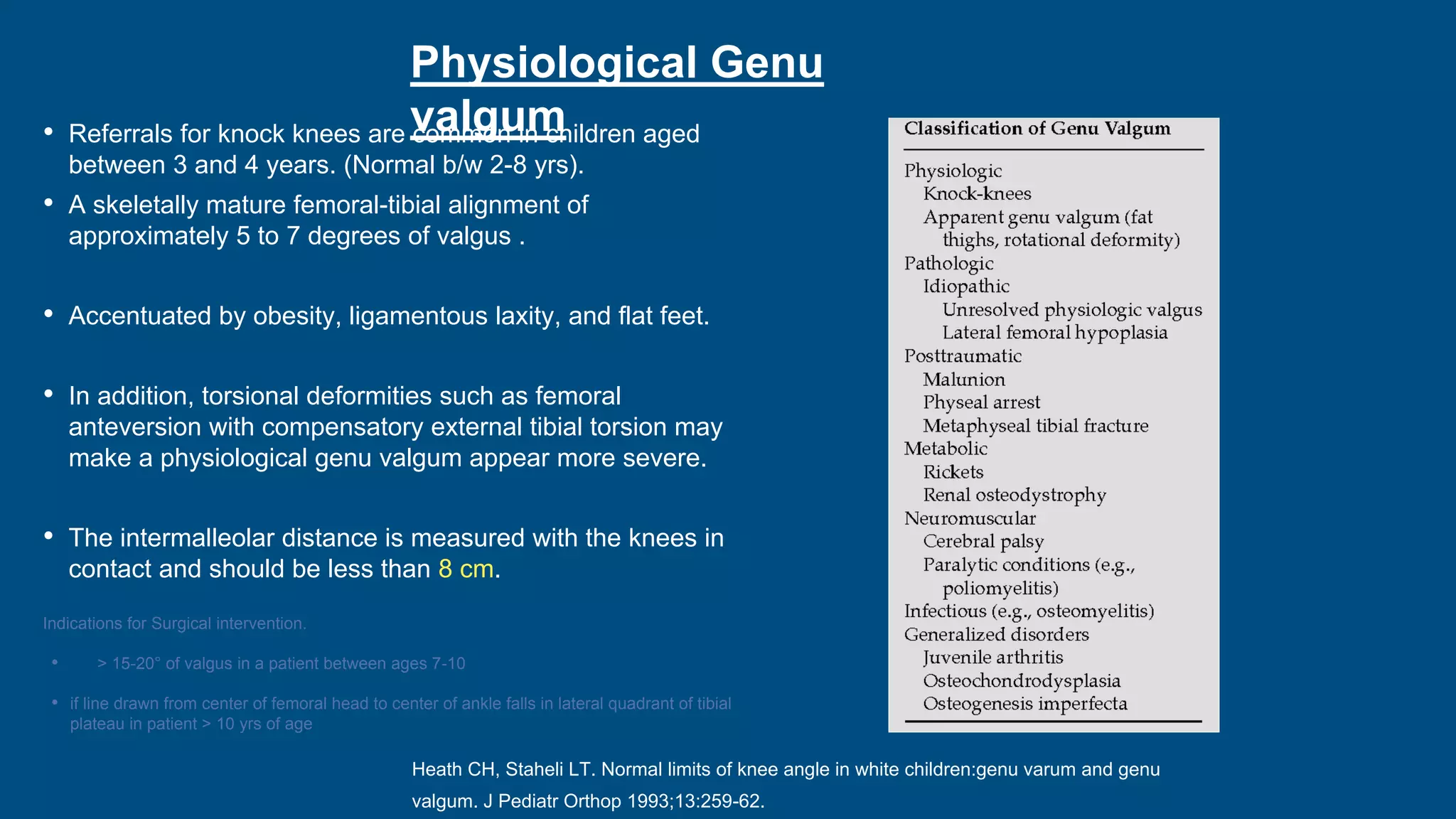
- Genu varum is normal in infants under 18 months while genu valgum peaks between 3-4 years and also typically resolves by age 7 without intervention.






























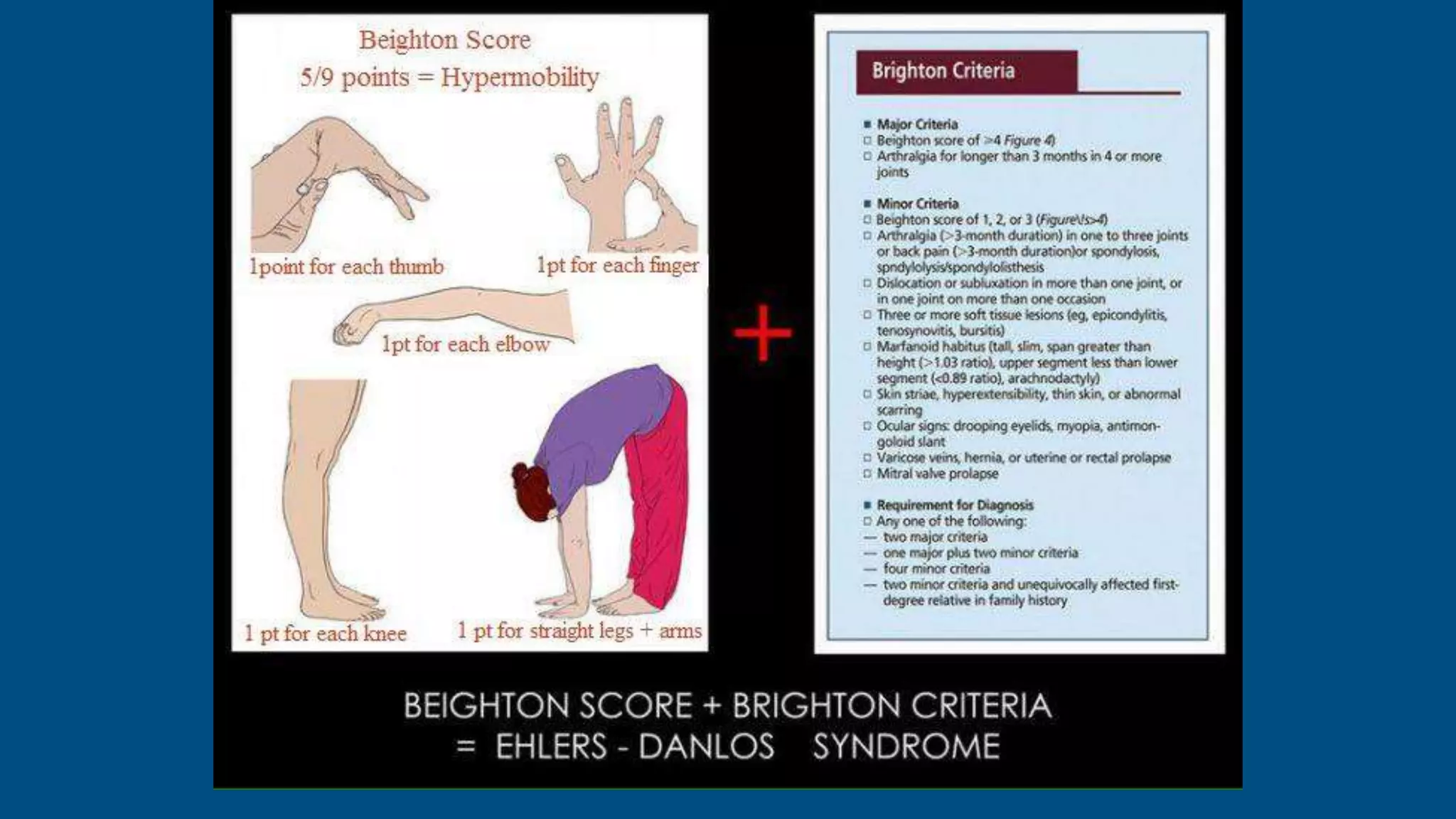
![prevalence of hypermobility in children as a phenomenon [as
opposed to joint hypermobility syndrome (JHS), i.e. symptomatic
hypermobility] depending on the age or ethnicity of the study
population or the inclusion criteria, has been reported to be
between 2.3 and 30%
Numerous extra-articular manifestations of JHS
have been similarly reported in children,
including
• chronic constipation and encopresis, enuresis
and urinary tract infections (UTI)
• higher skin extensibility
• lower systemic blood pressure
• lower bone quantitative ultrasound
measurements
• chronic fatigue syndrome
• temporomandibular joint disease
• fibromyalgia
• gross motor developmental delay](https://image.slidesharecdn.com/normalvariationsinchildren-211029163454/75/Normal-variations-in-children-44-2048.jpg)


