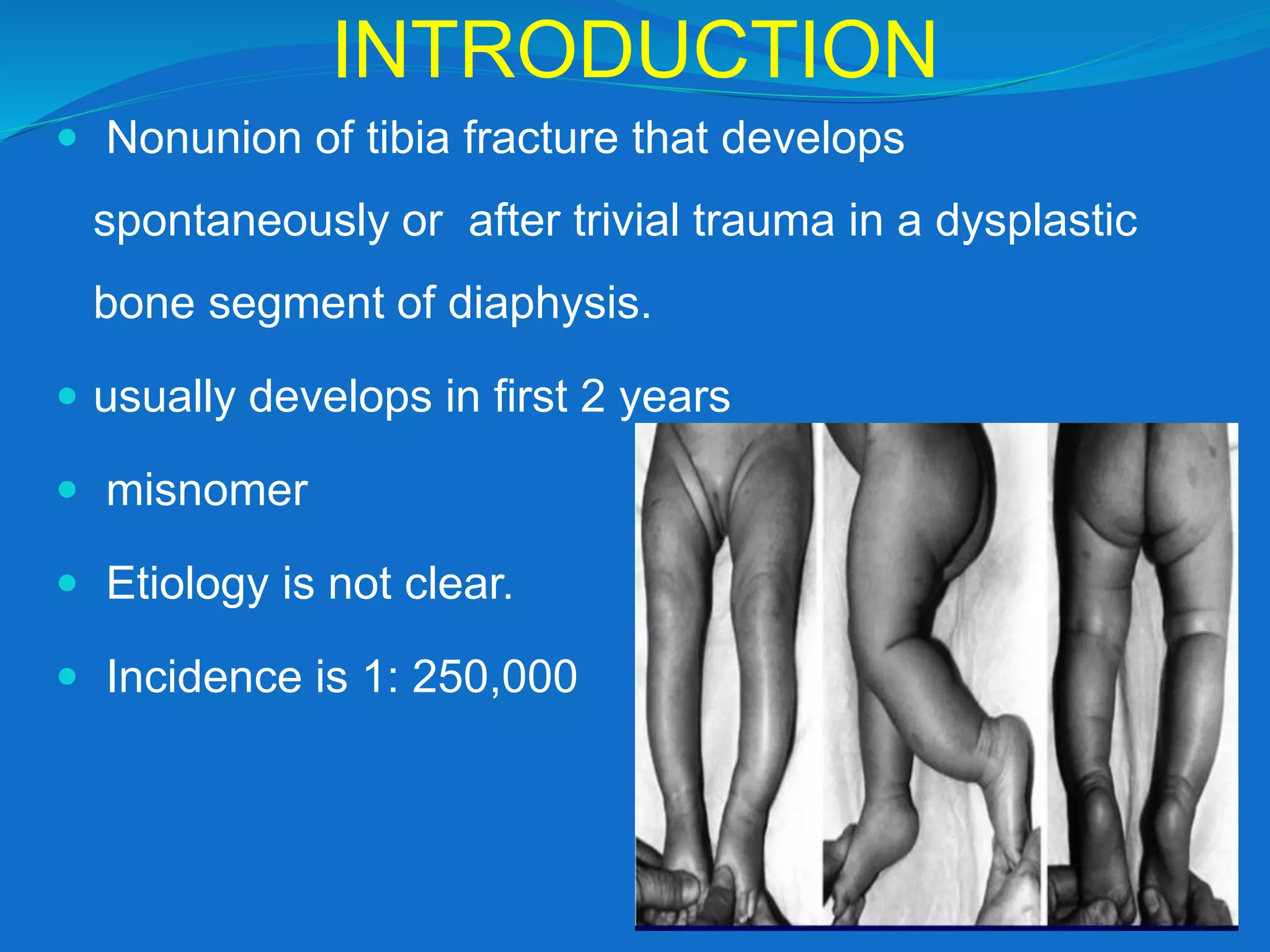
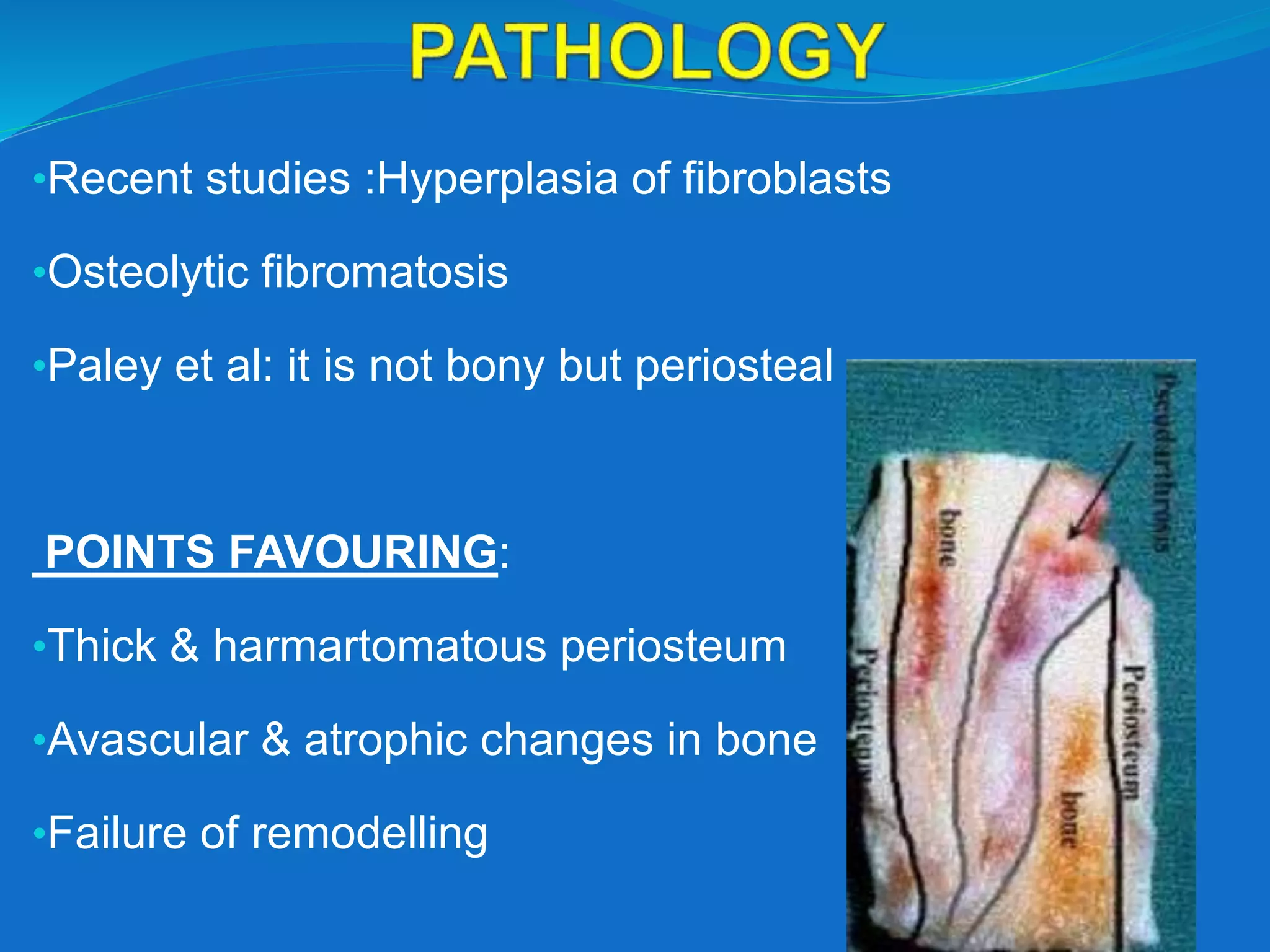
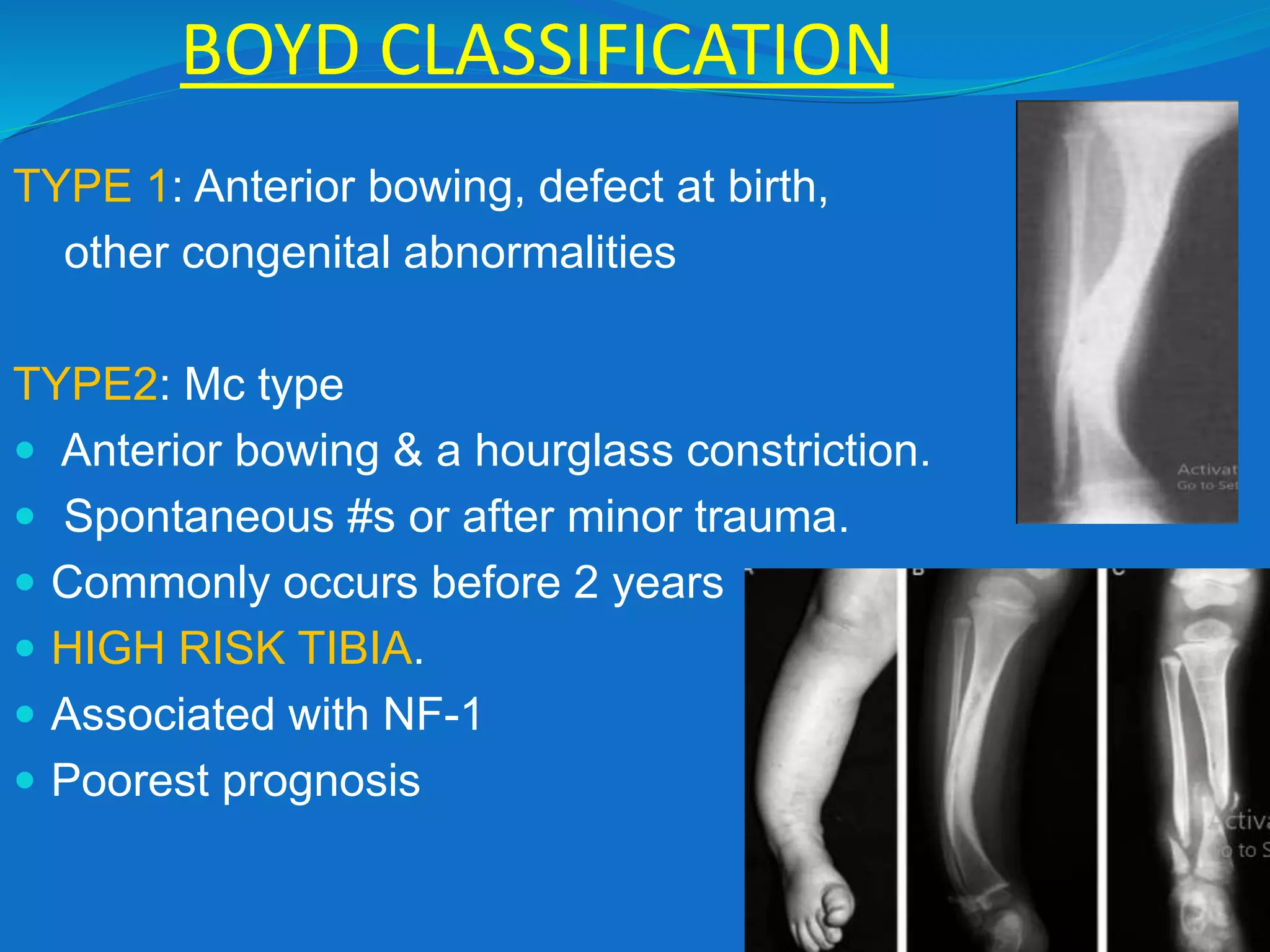
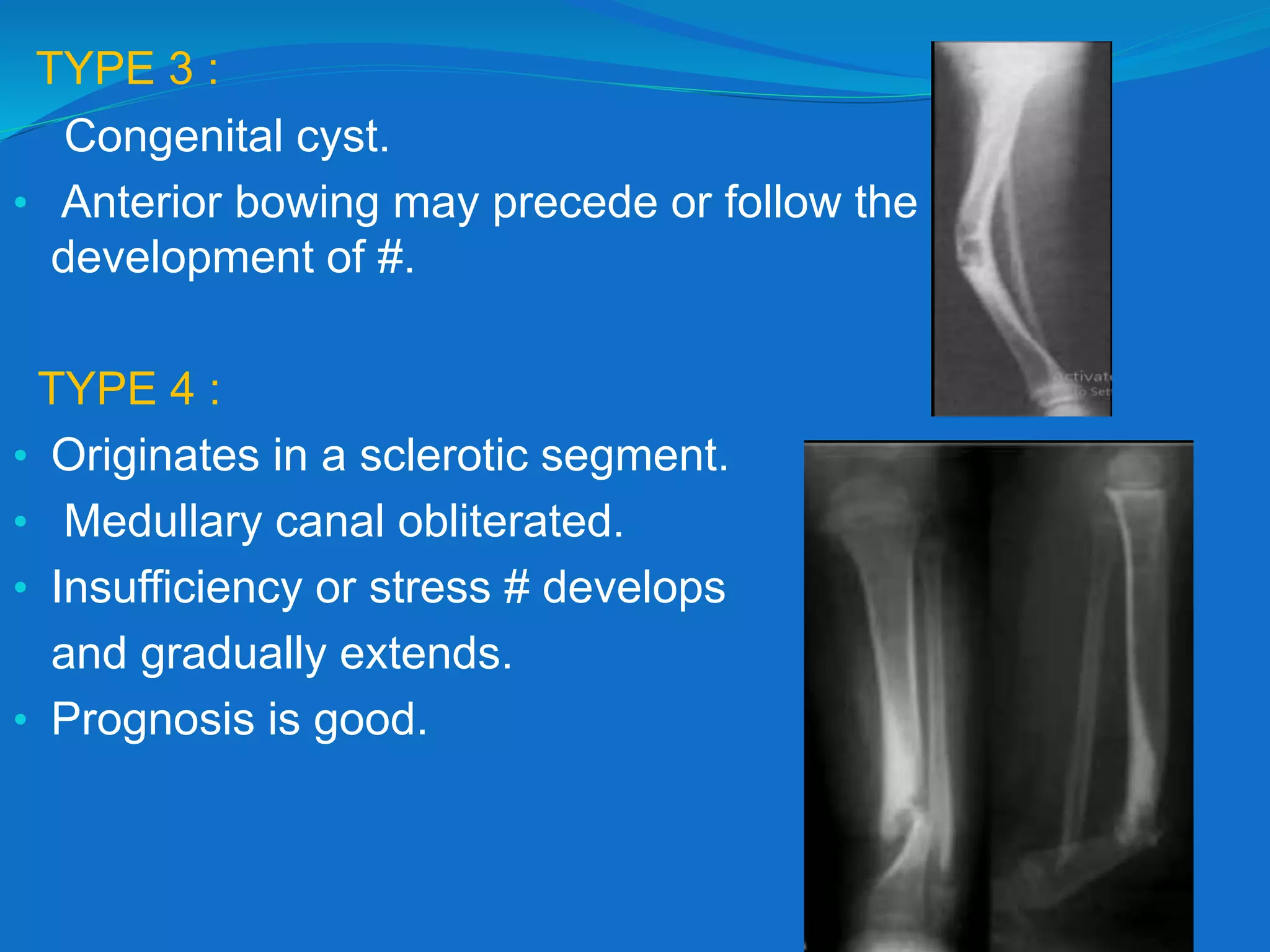
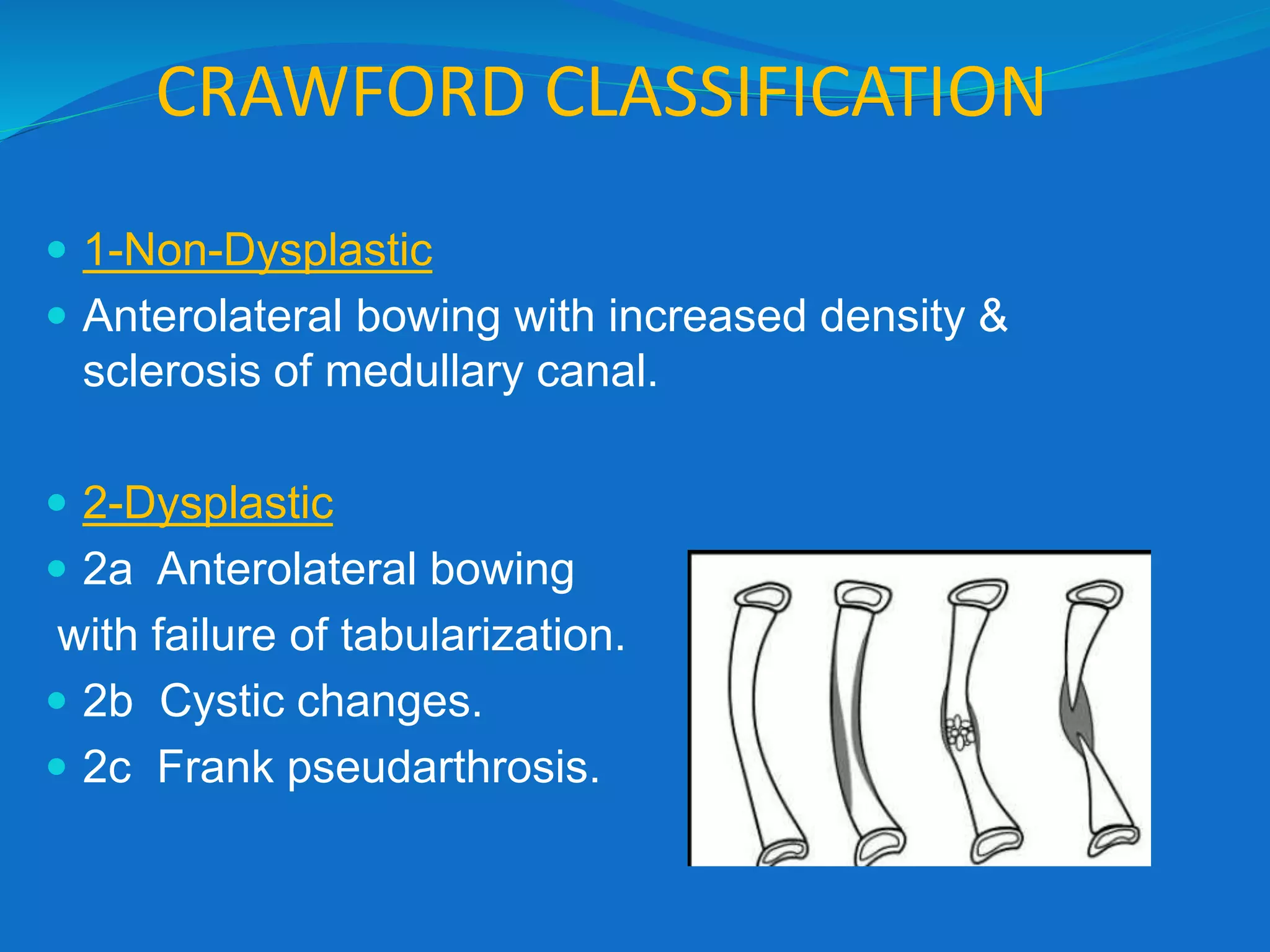
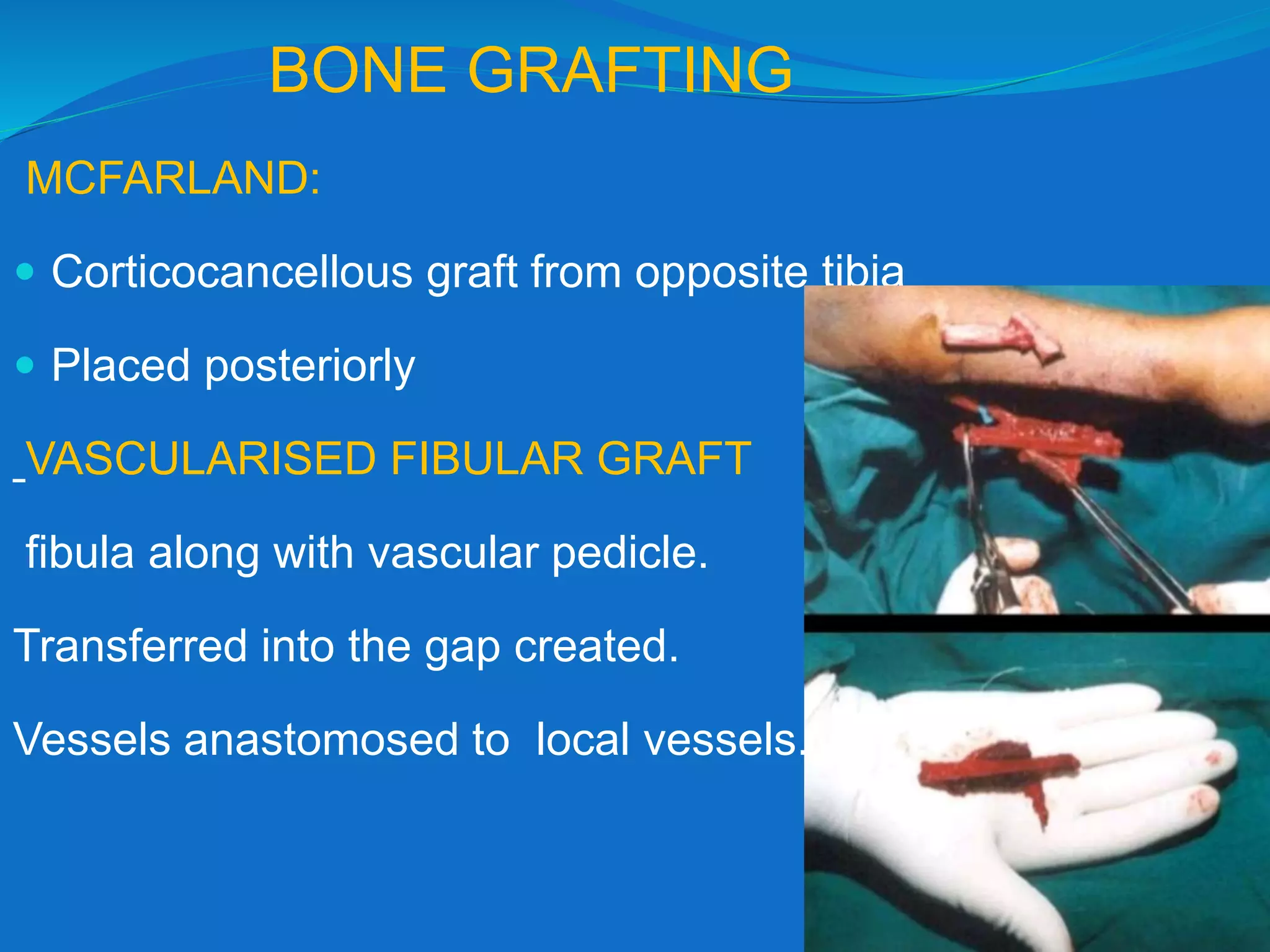
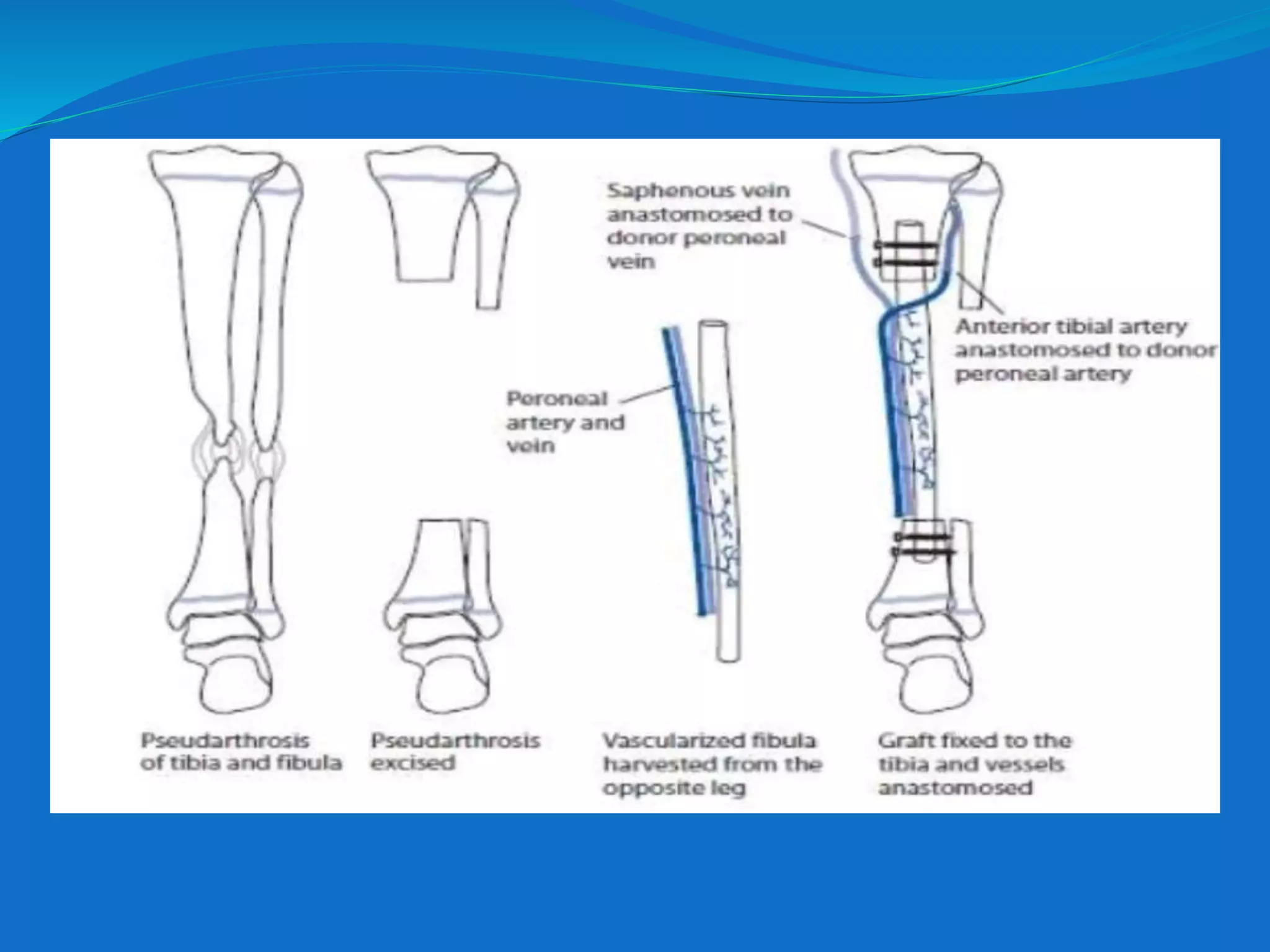
This document discusses congenital pseudarthrosis of the tibia (CPT), a rare bone condition where the tibia fails to heal properly. It has a strong association with neurofibromatosis type 1. The document covers the etiology, classification systems, diagnosis, and treatment options for CPT. Treatment aims to achieve union of the tibia, prevent refracture, correct limb length discrepancy, and prevent ankle deformities. Surgical techniques discussed include bone grafting, intramedullary fixation, the Ilizarov technique, and bone morphogenetic proteins. Complications can include refracture, malalignment, limb length discrepancy, and ankle issues.