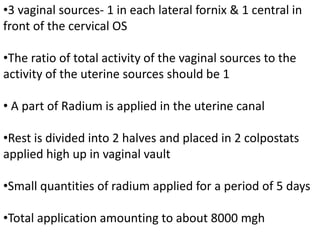
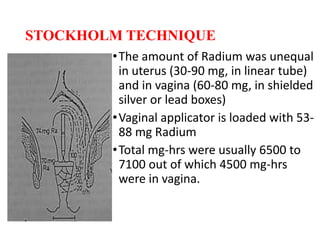
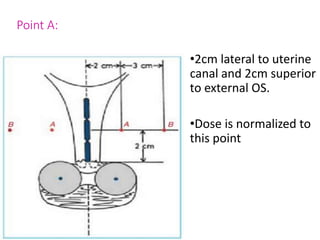
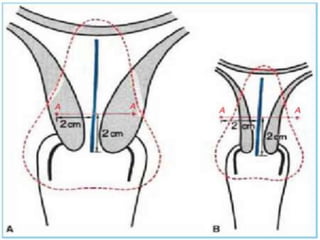
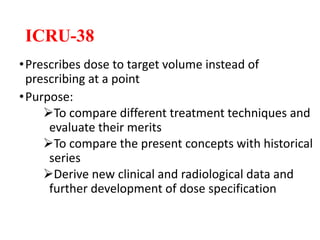
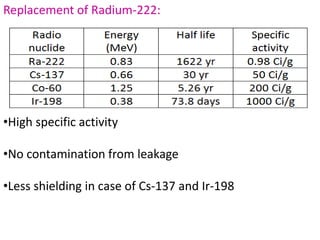
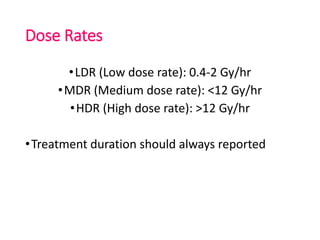
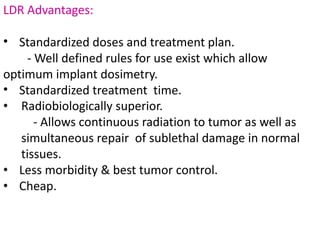
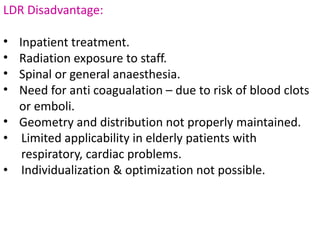
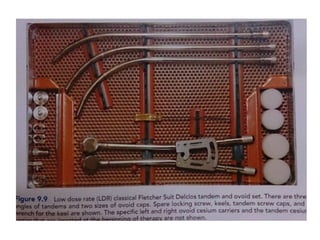
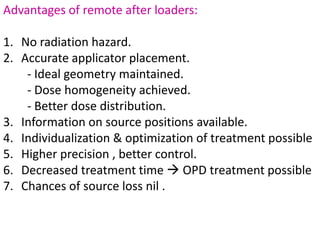
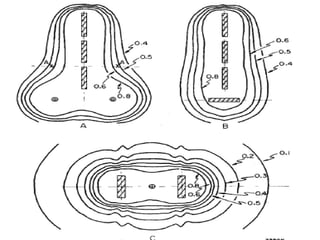
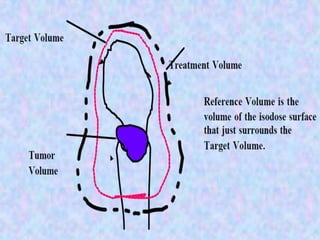
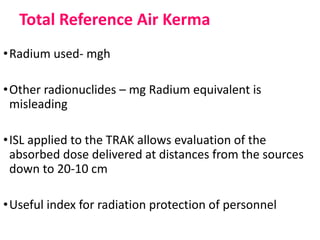
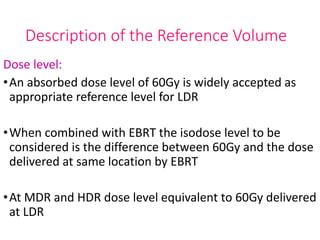
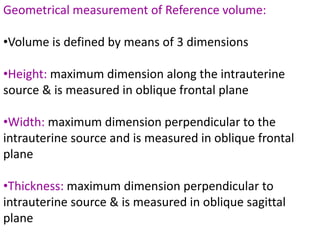
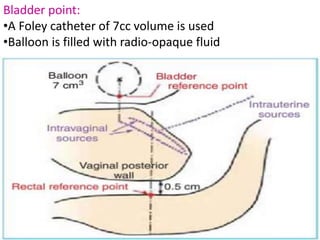
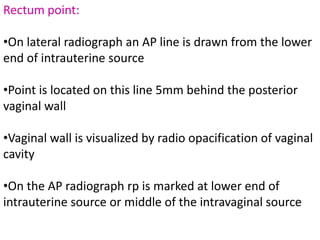
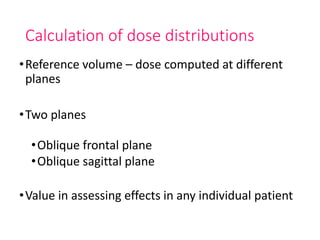
This document discusses Intra-cavitary Brachytherapy (ICBT) for treating cervical cancer. It describes different historical ICBT systems like Paris, Stockholm, and Manchester systems. It also discusses modern techniques like remote afterloaders and recommendations for reporting absorbed doses and volumes in ICBT. Key points include different dose rates (LDR, MDR, HDR), advantages of remote afterloaders in maintaining geometry and dose distribution, and recommending specifying absorbed dose to the target volume rather than at a single point for ICBT.