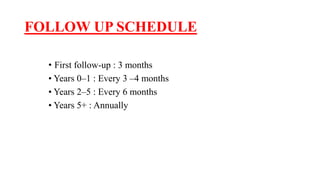
This document provides guidelines for the management of prostate carcinoma. It discusses risk stratification, treatment options including active surveillance, radiation therapy techniques, brachytherapy, adjuvant radiation, androgen deprivation therapy, and follow-up schedules. Treatment is tailored based on risk level (very low, low, intermediate, high, very high risk) and life expectancy. Image-guided radiation therapy allows for daily adjustment of patient positioning and beam targeting. Androgen deprivation therapy is an important part of treatment for intermediate to very high risk disease. Follow-up involves monitoring PSA levels at regular intervals post-treatment.