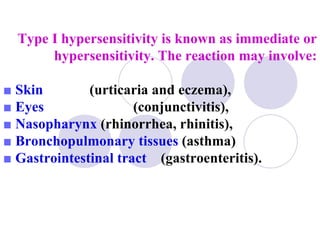
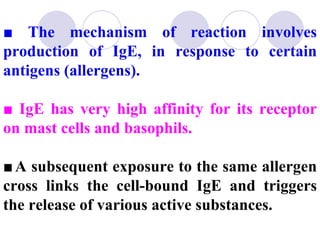
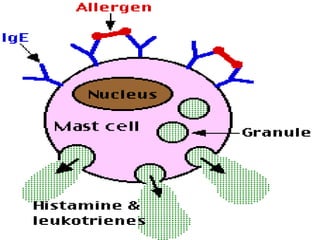
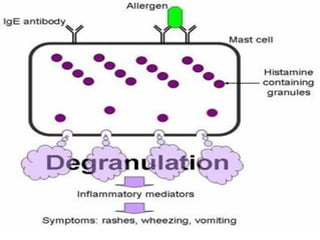
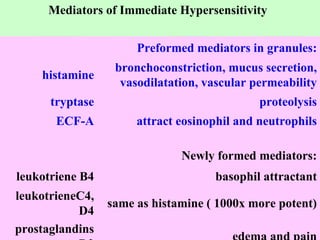
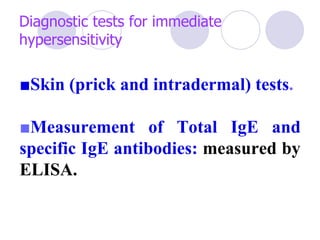
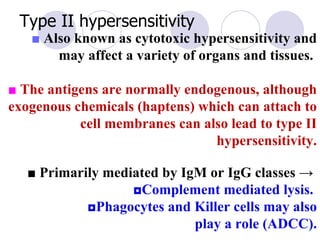
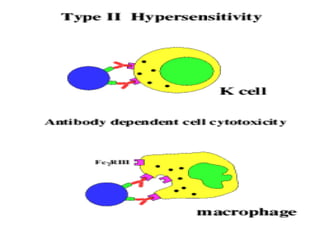
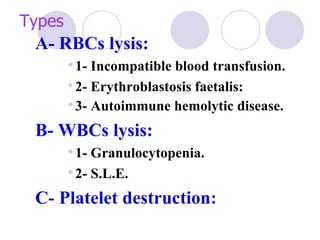
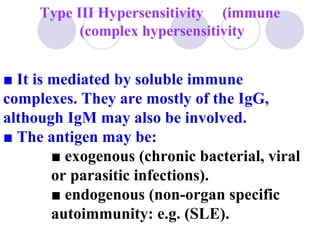
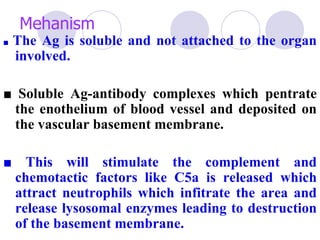
Hypersensitivity reactions are classified into four types. Type I is an immediate hypersensitivity mediated by IgE antibodies. Type II involves cytotoxic reactions against cell surfaces. Type III occurs when soluble antigens form complexes with antibodies. Type IV is a delayed hypersensitivity mediated by T cells and monocytes.