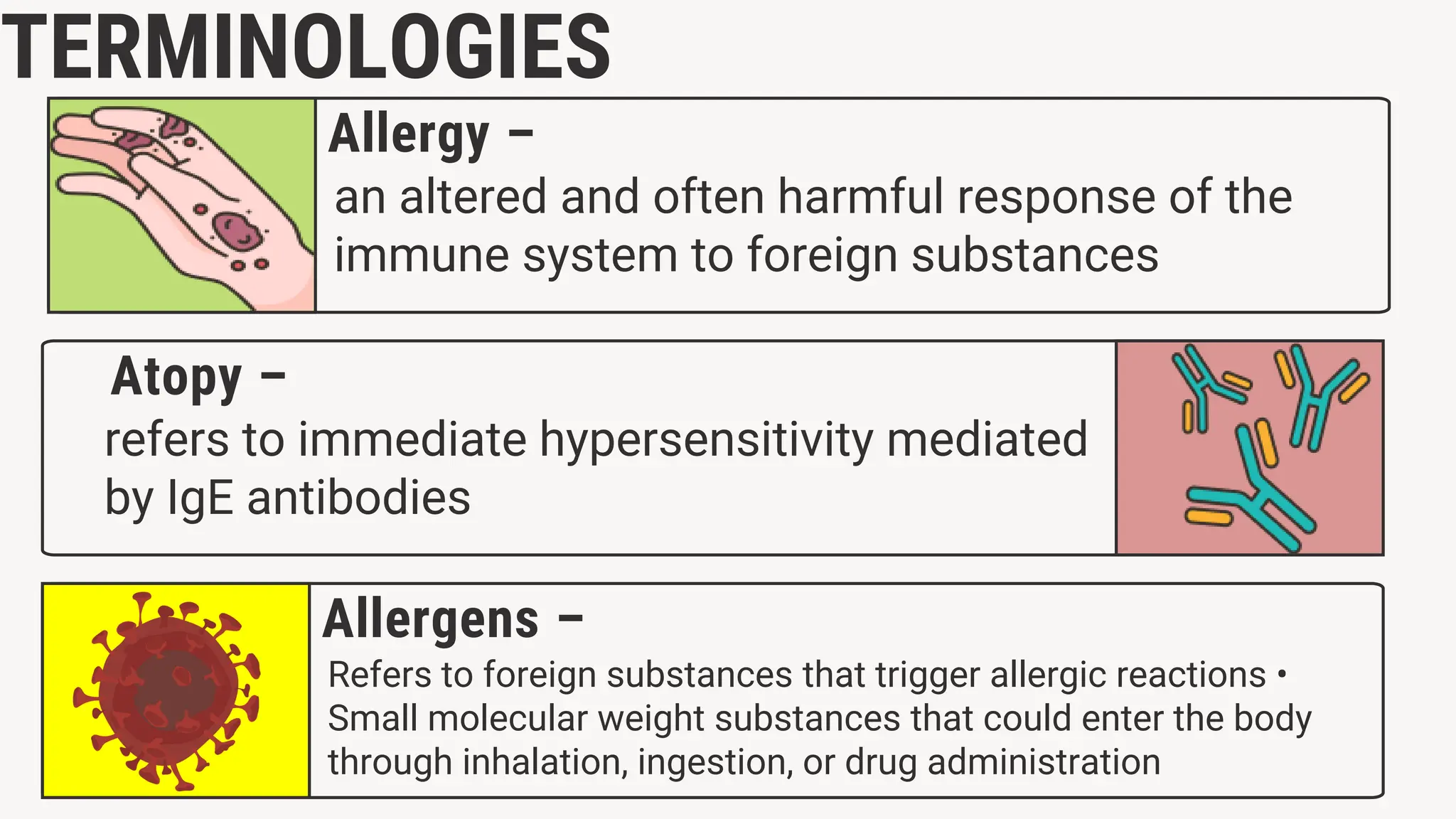
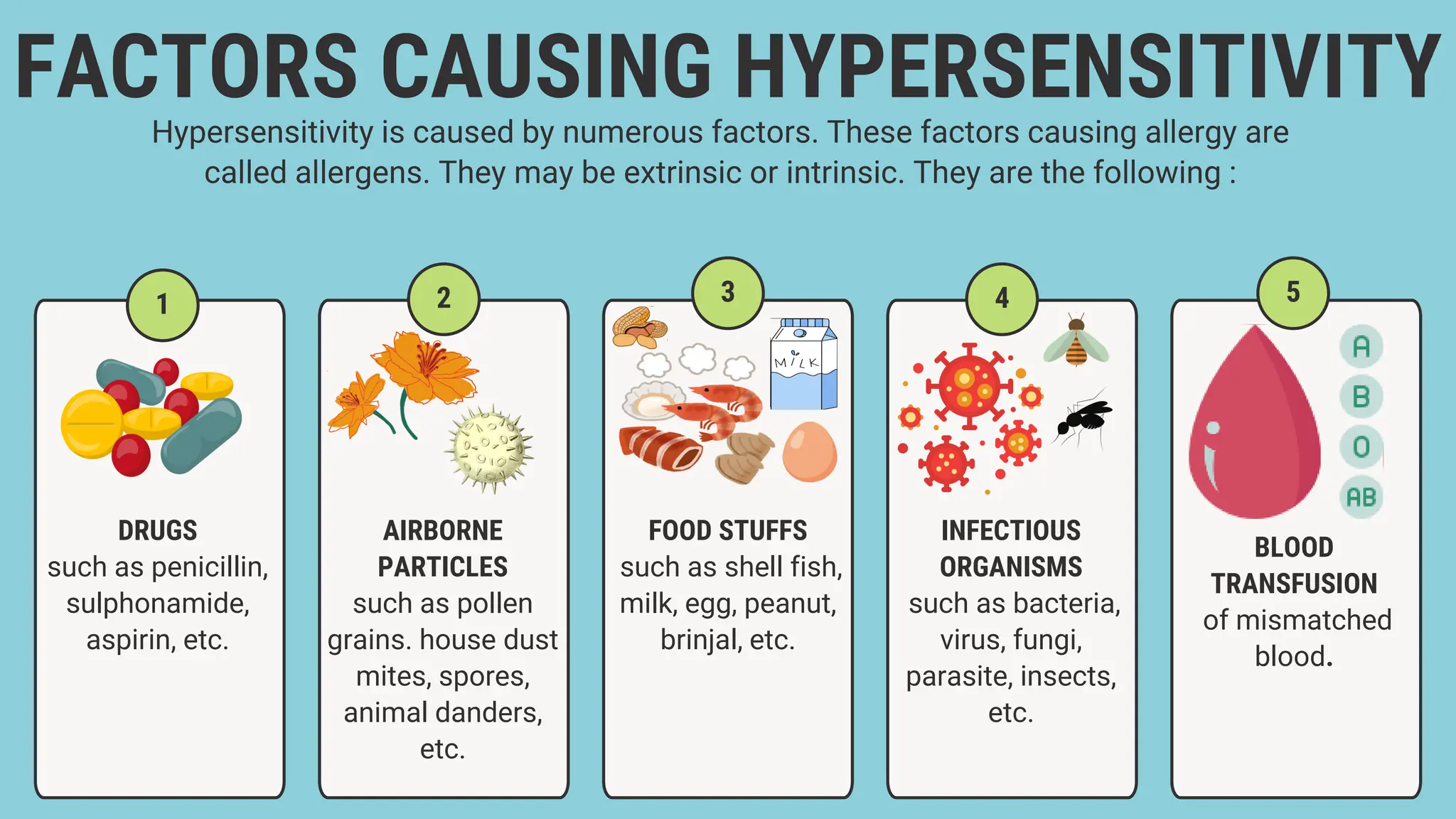
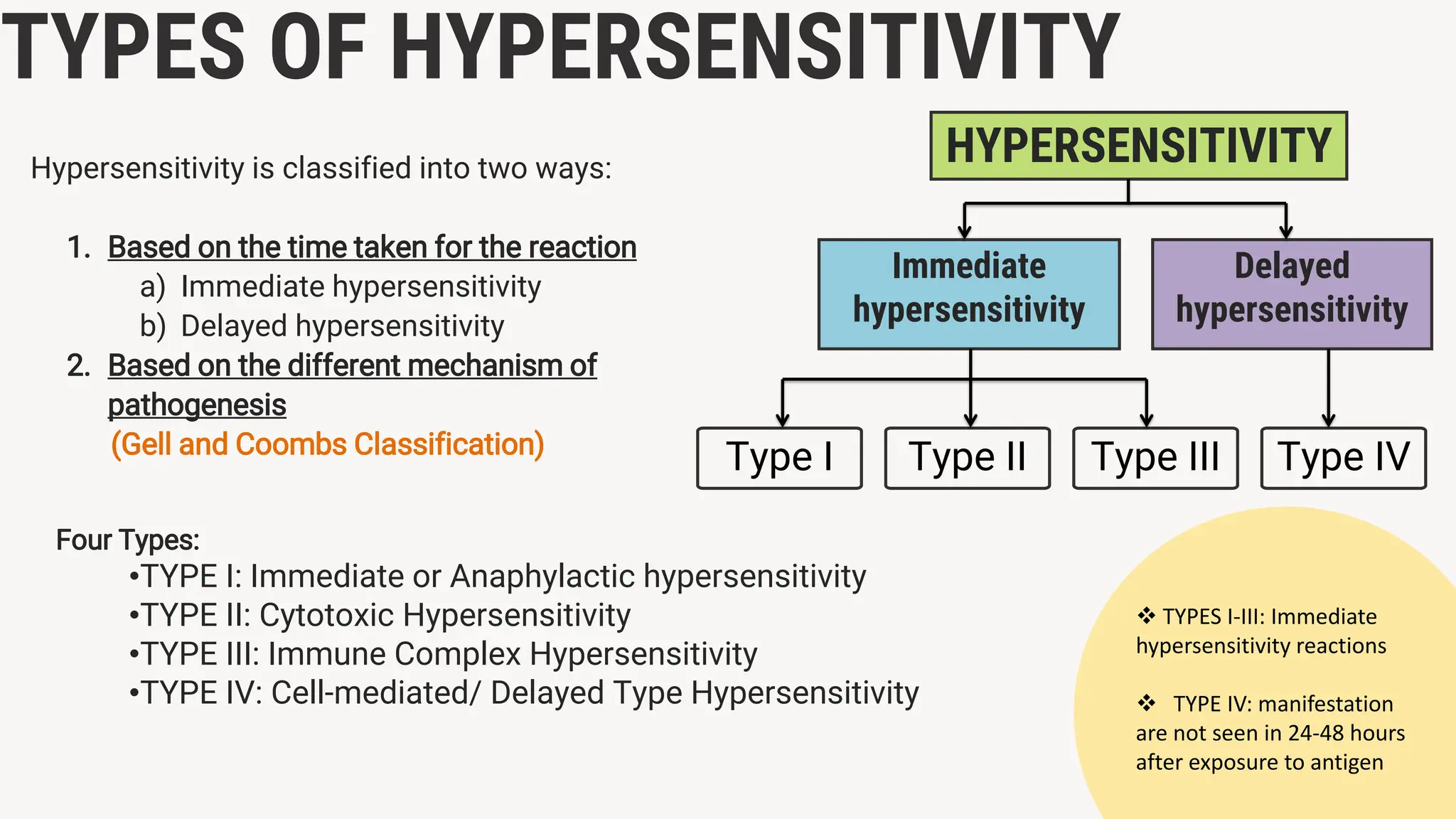
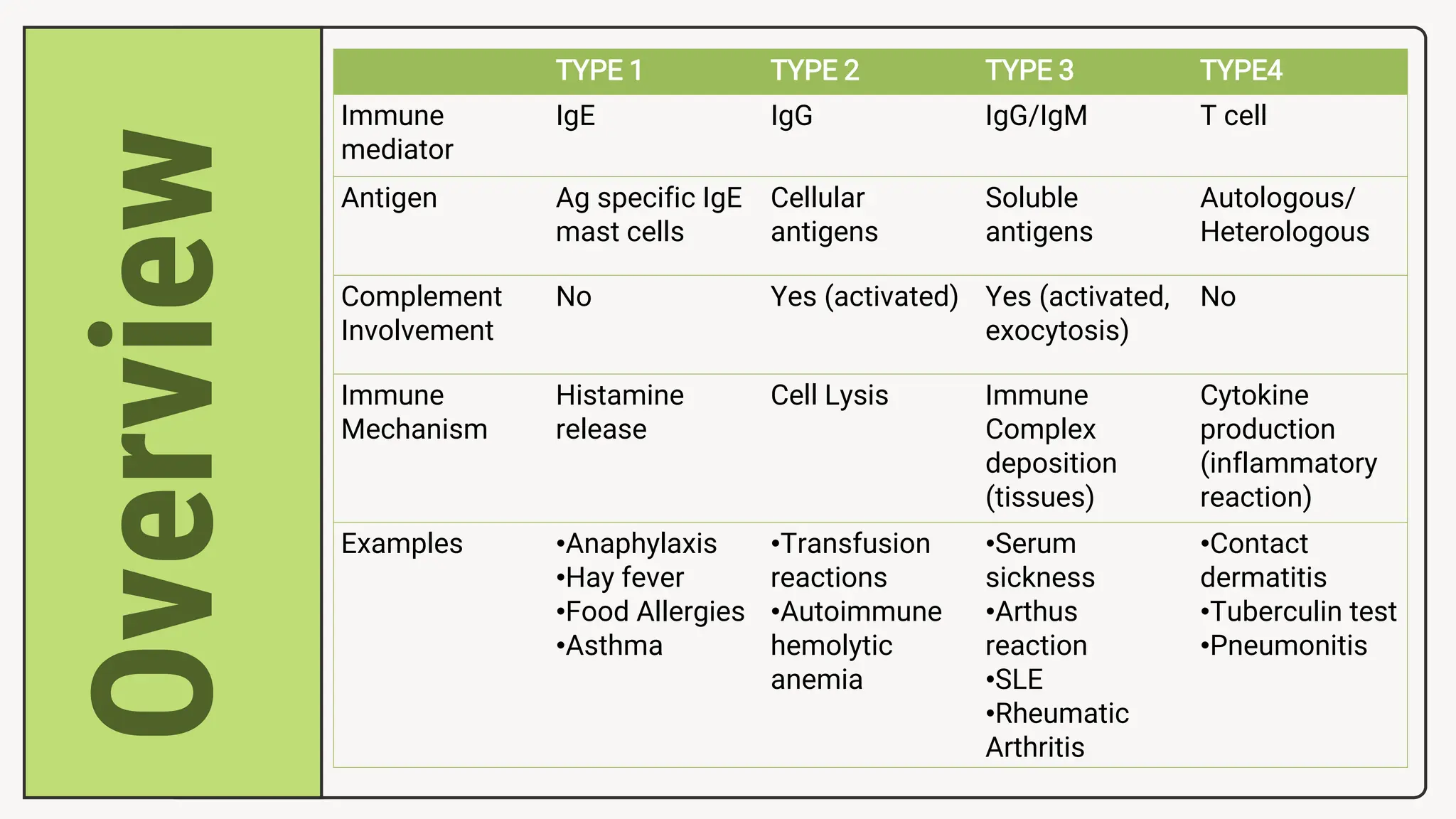
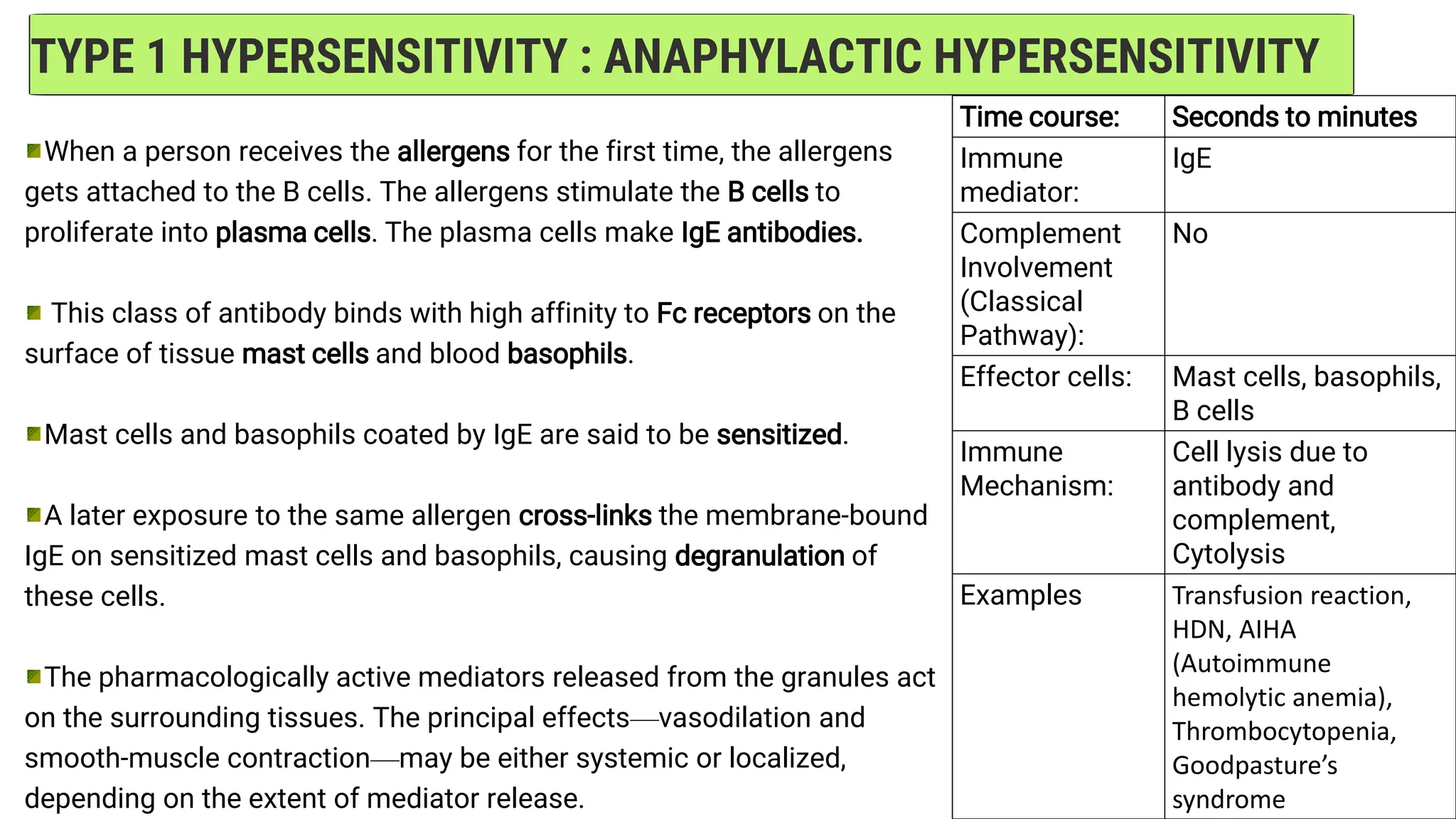
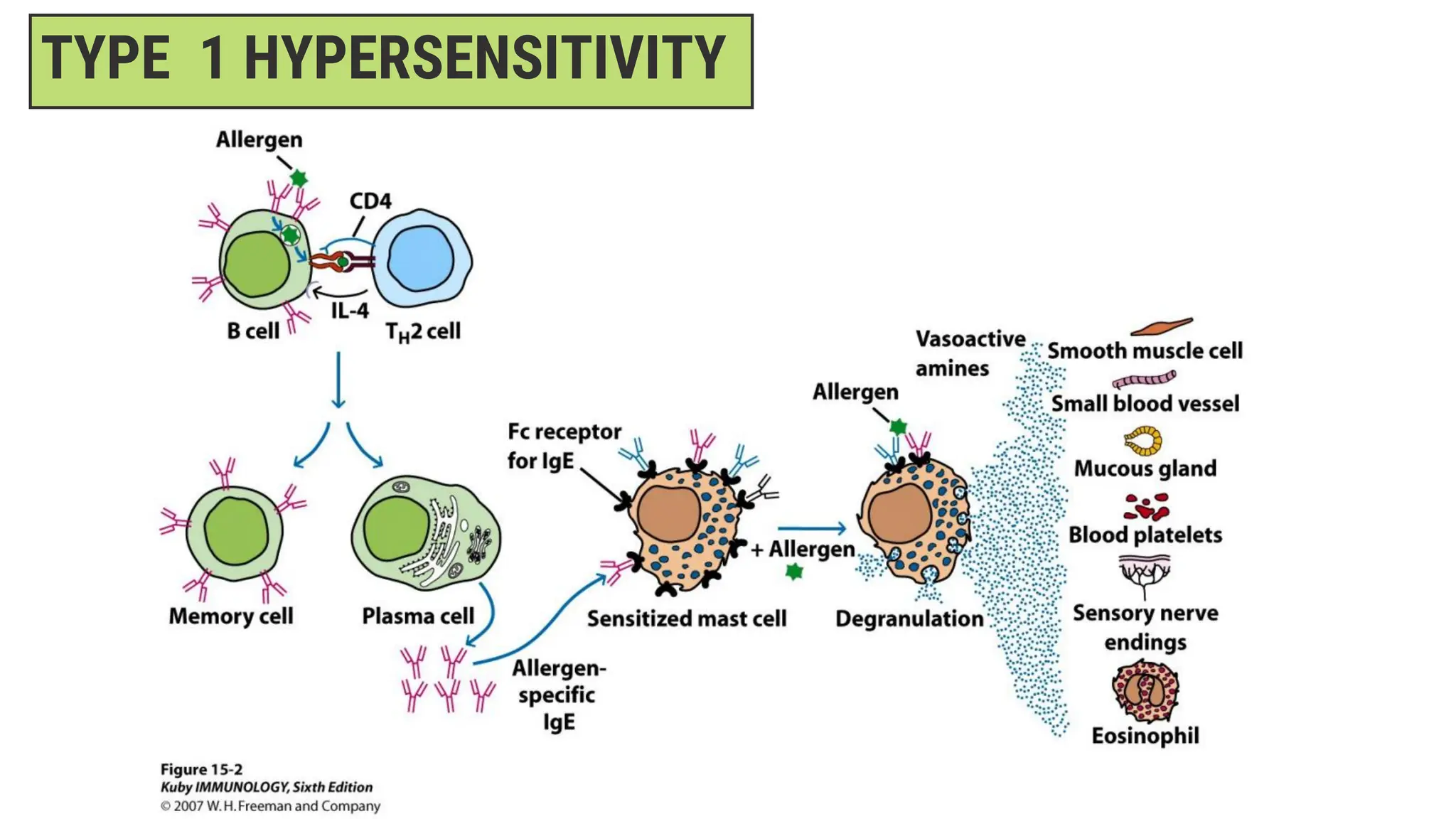
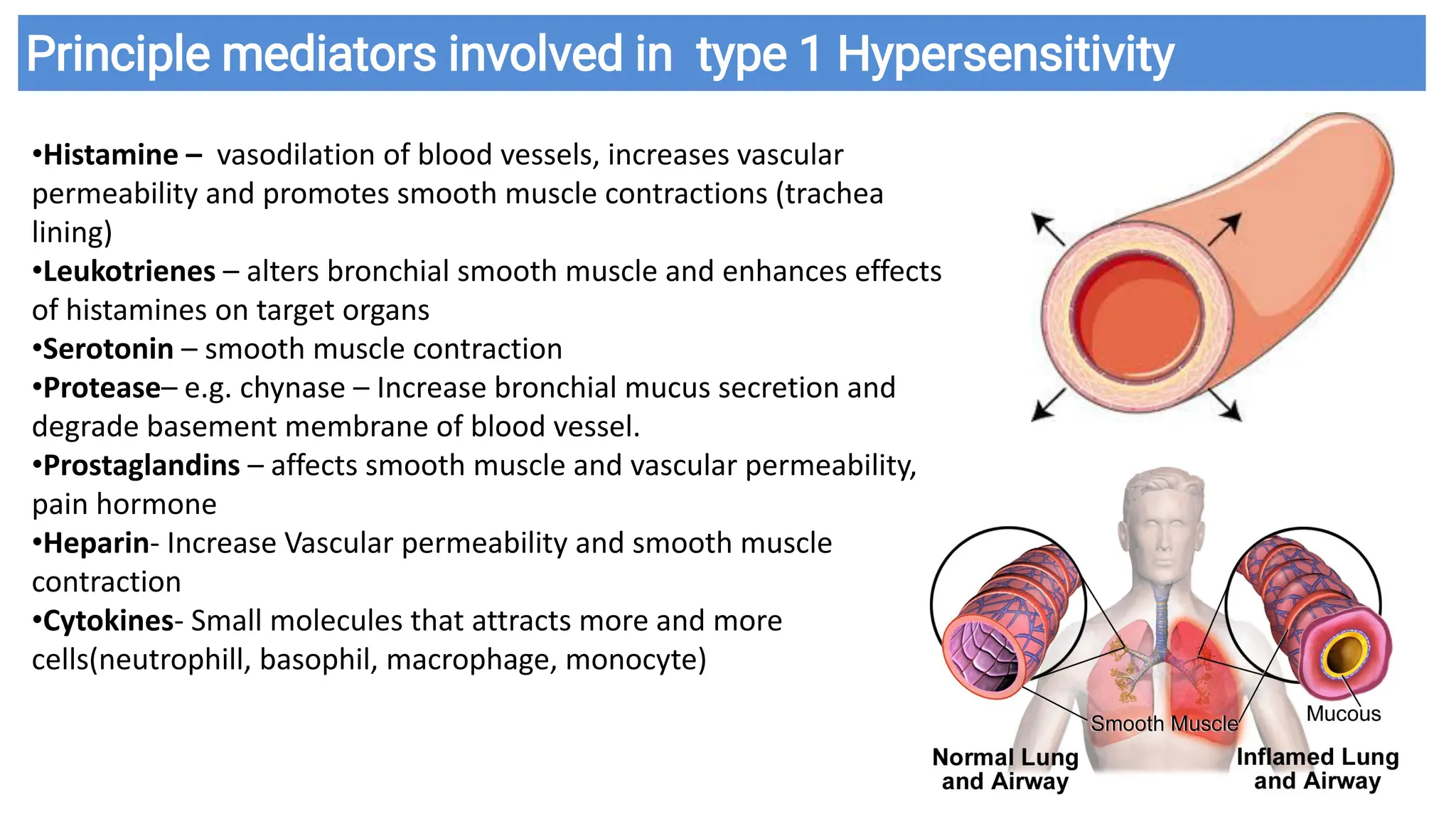
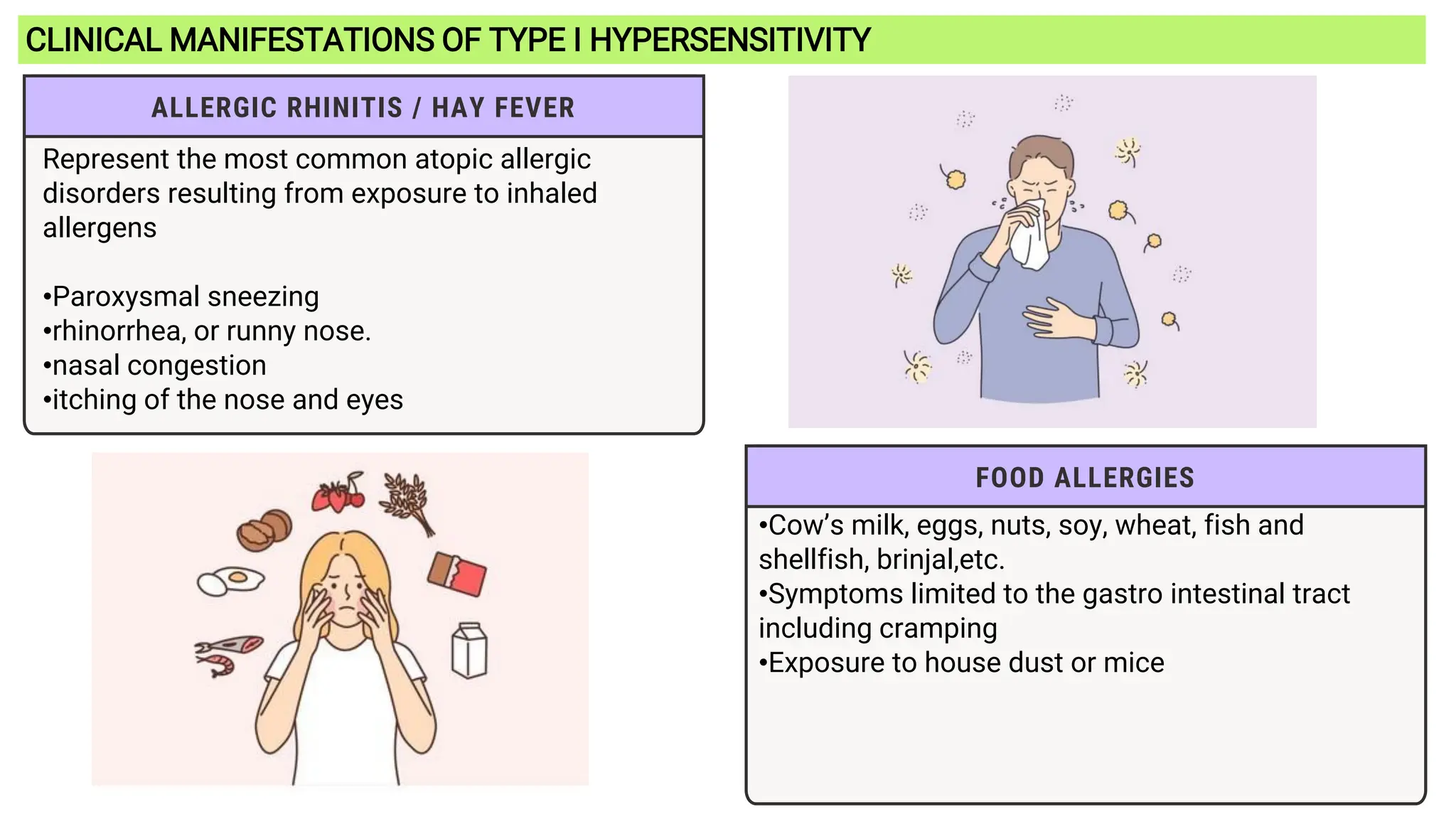
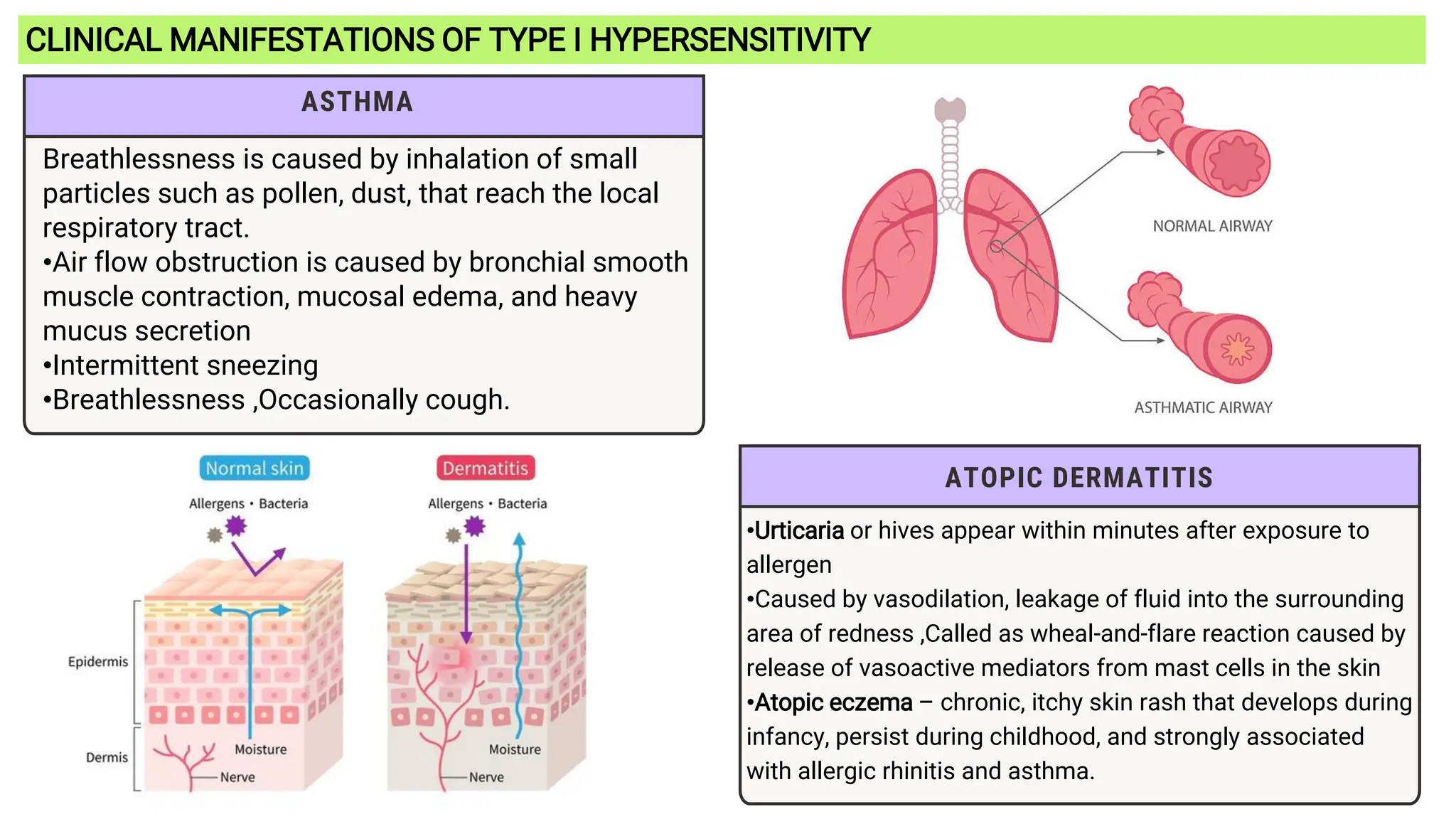
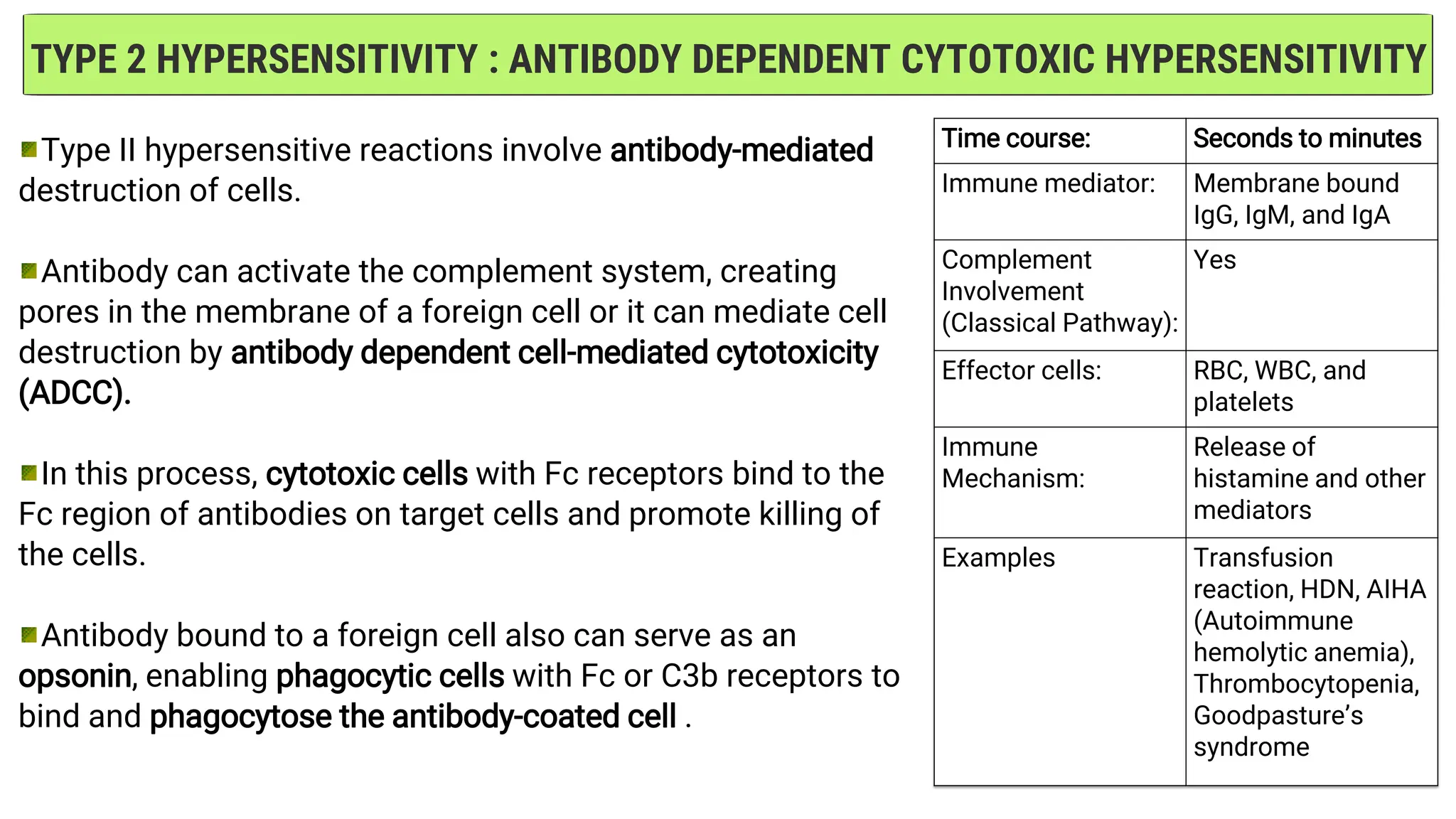
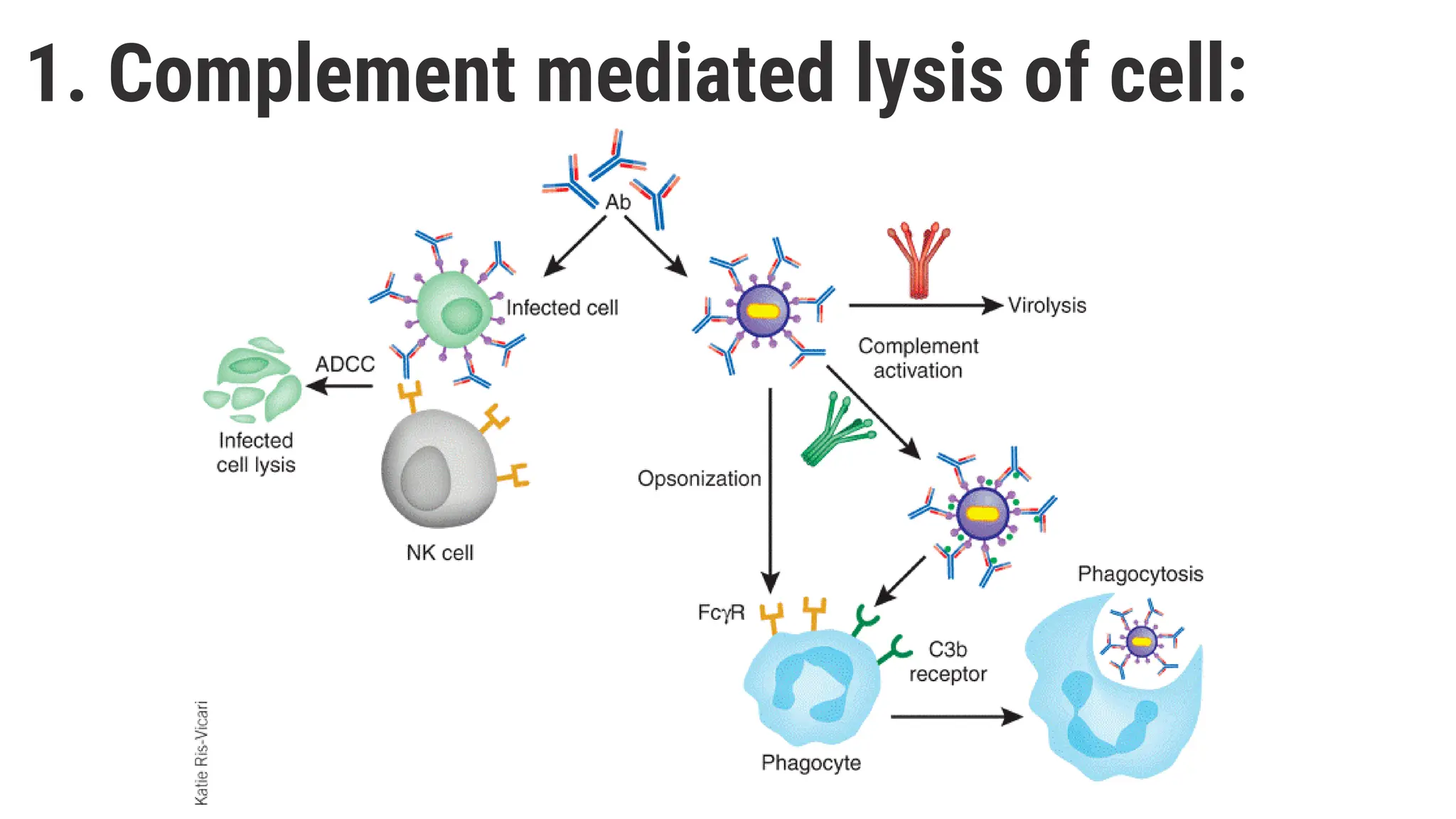
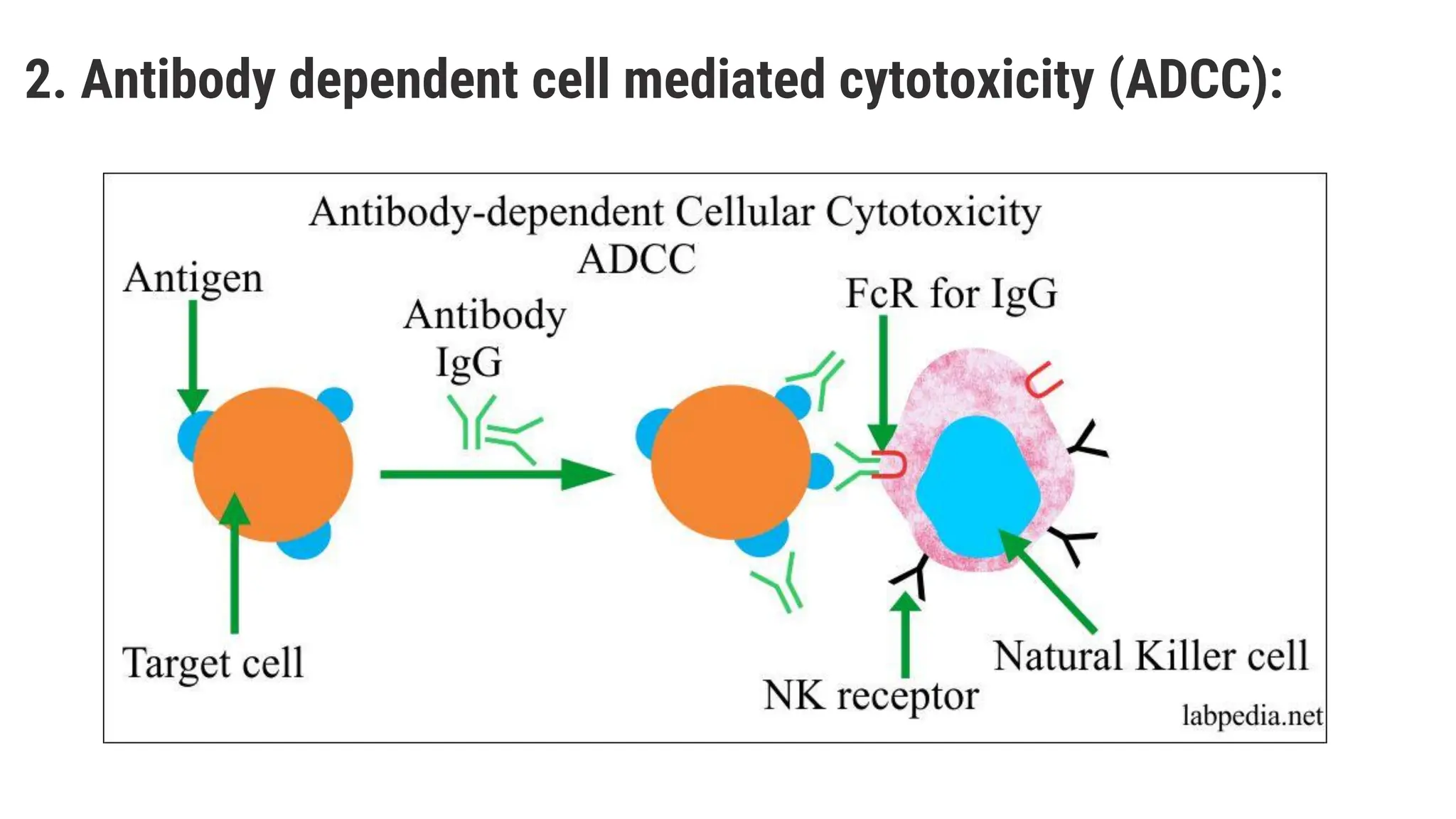
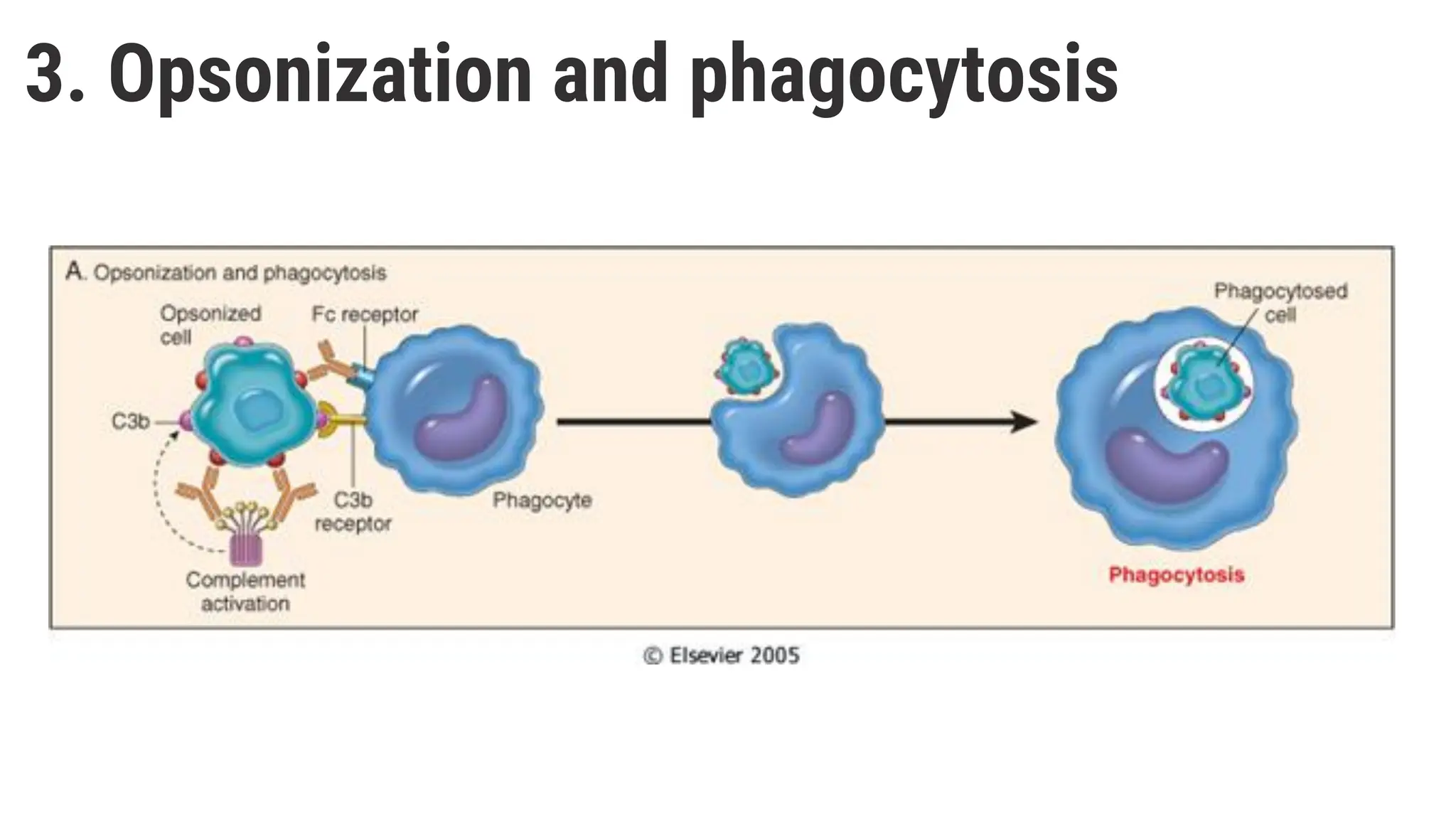
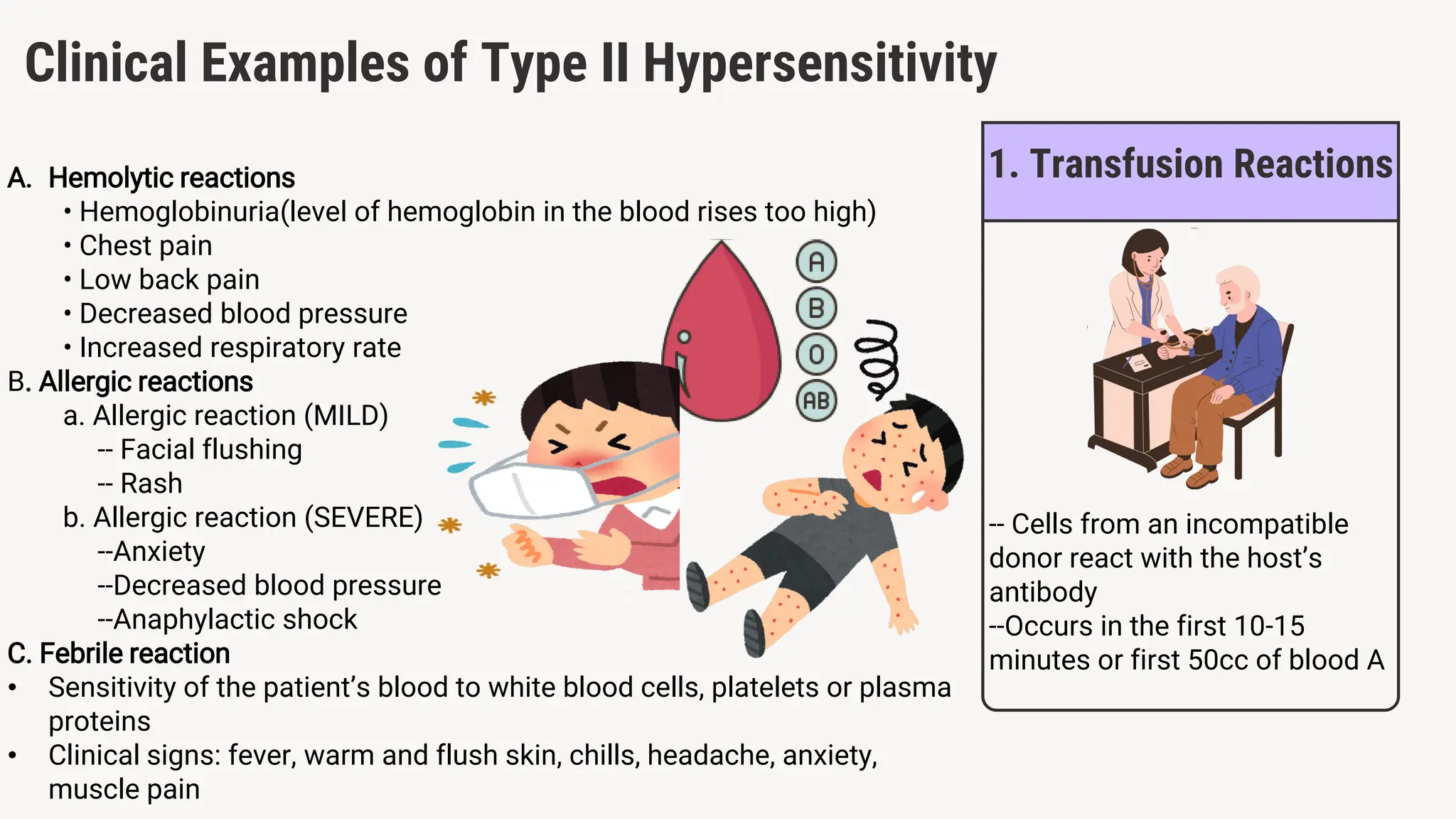
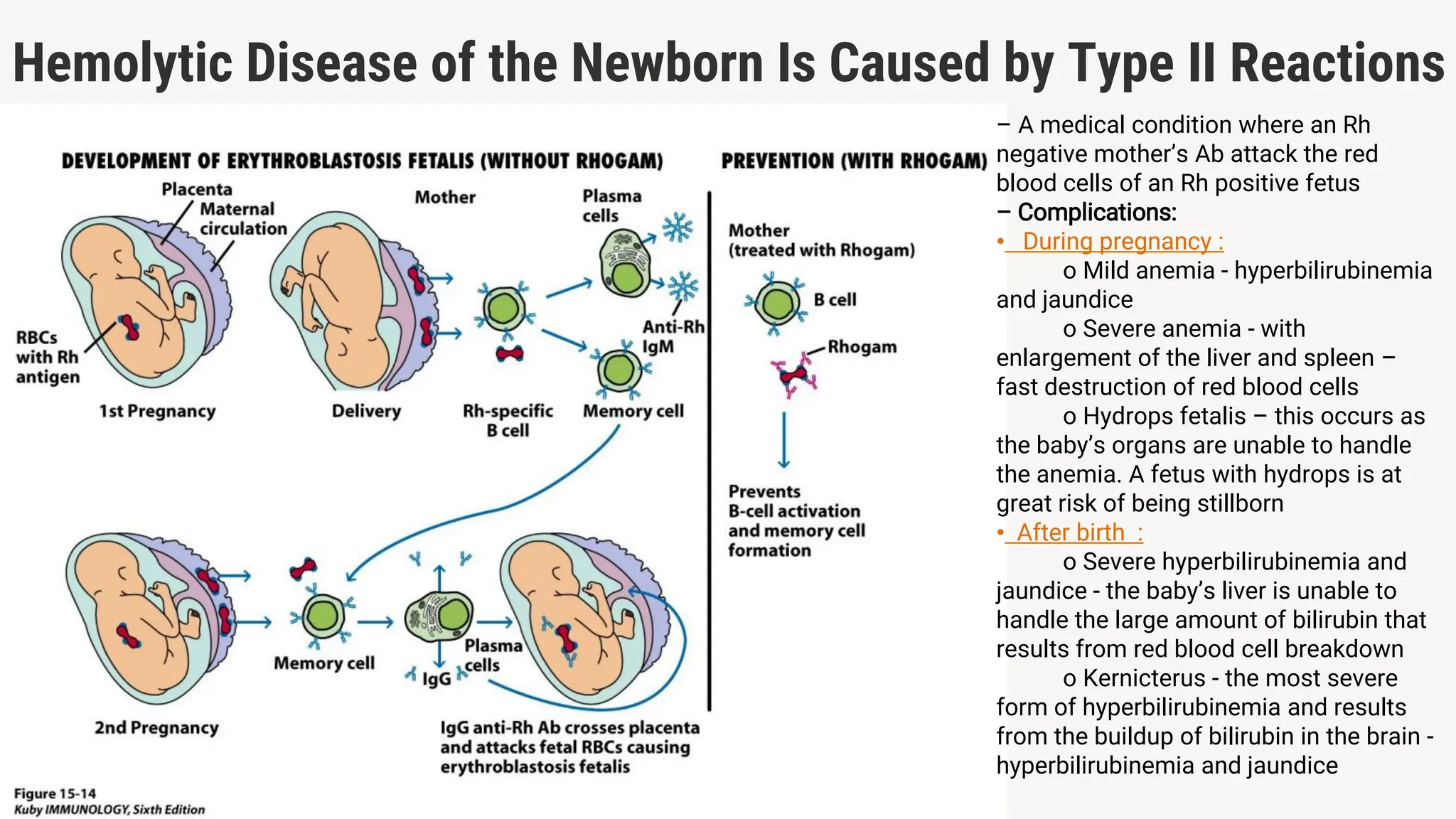
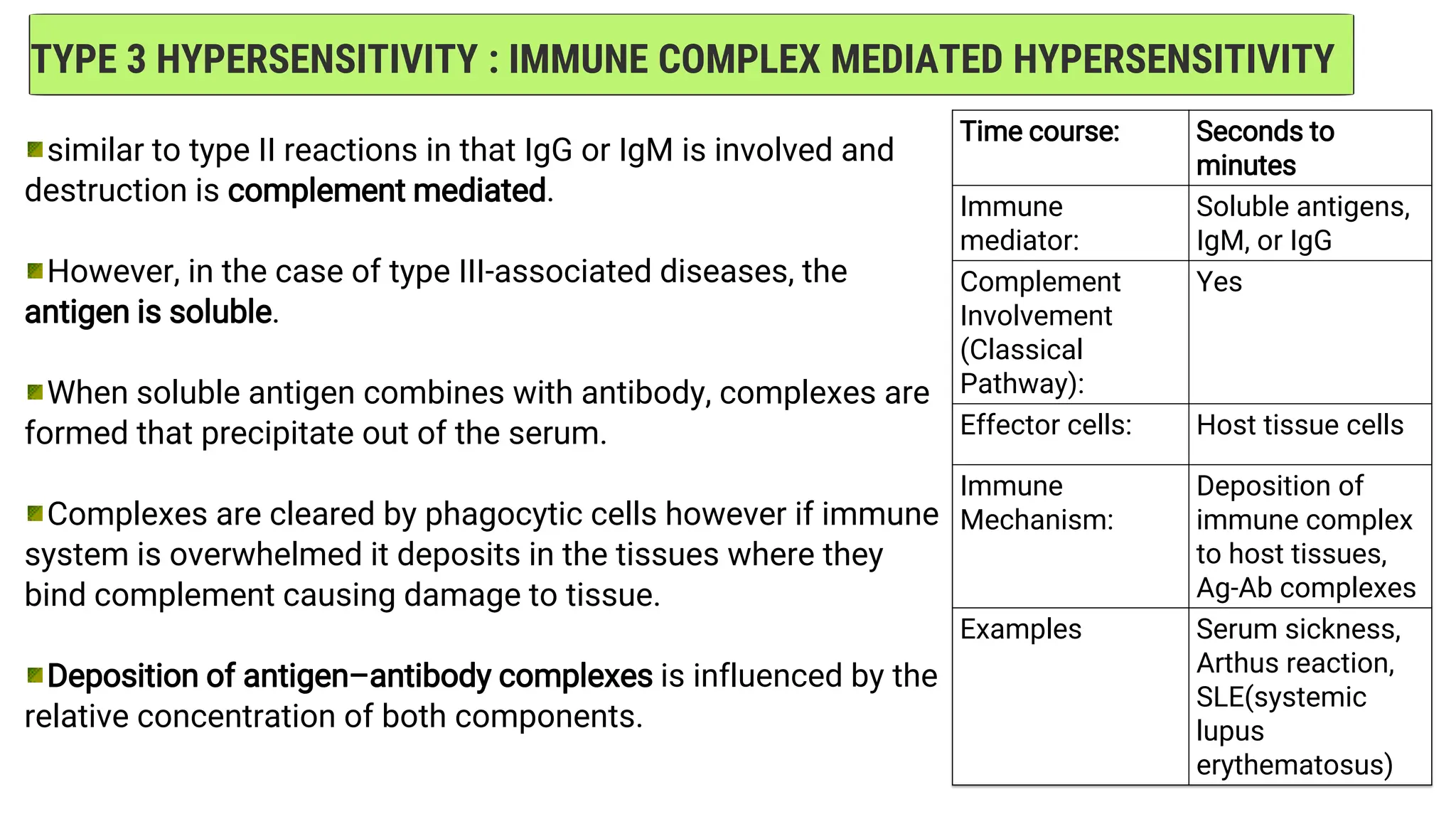
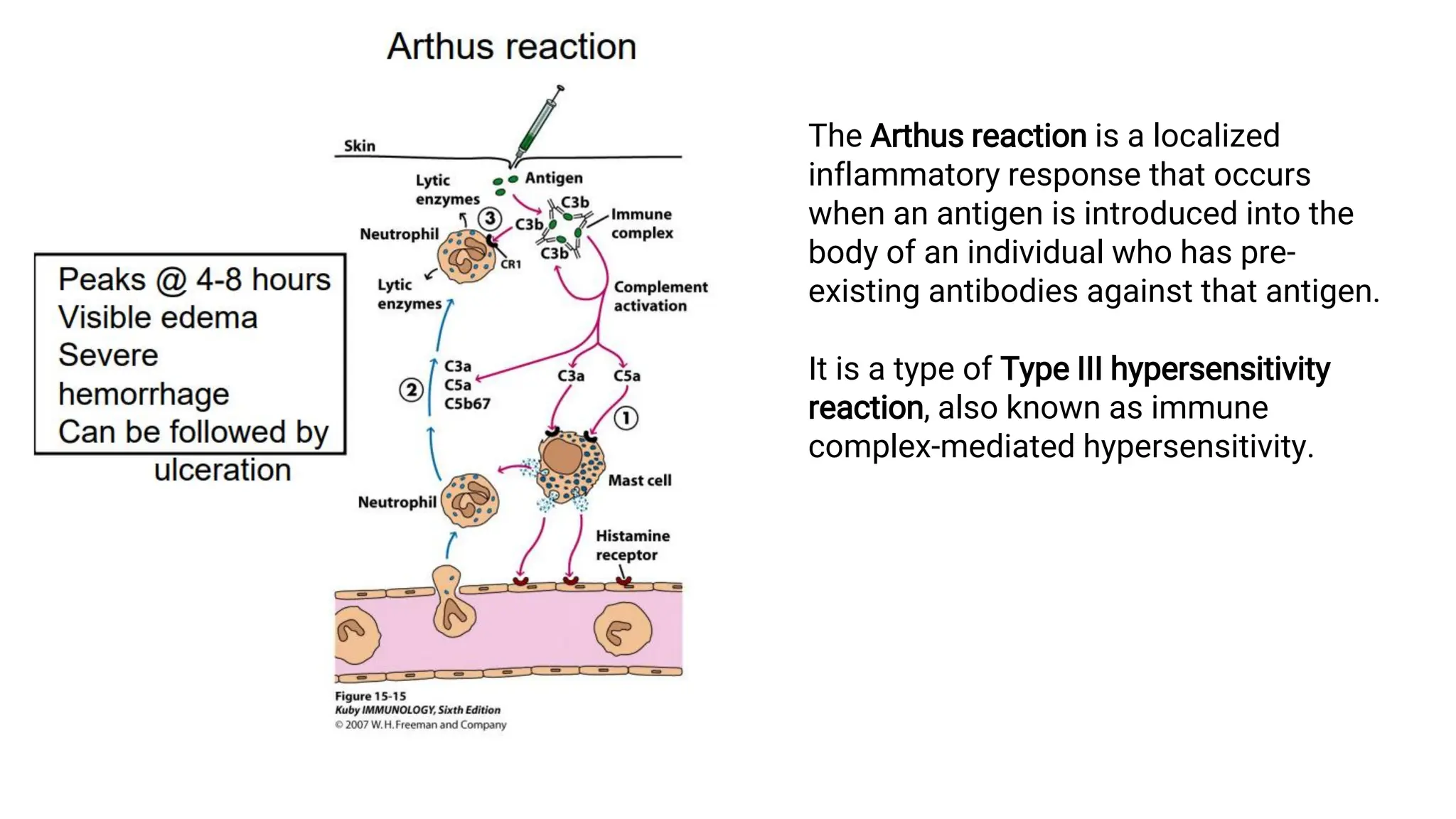
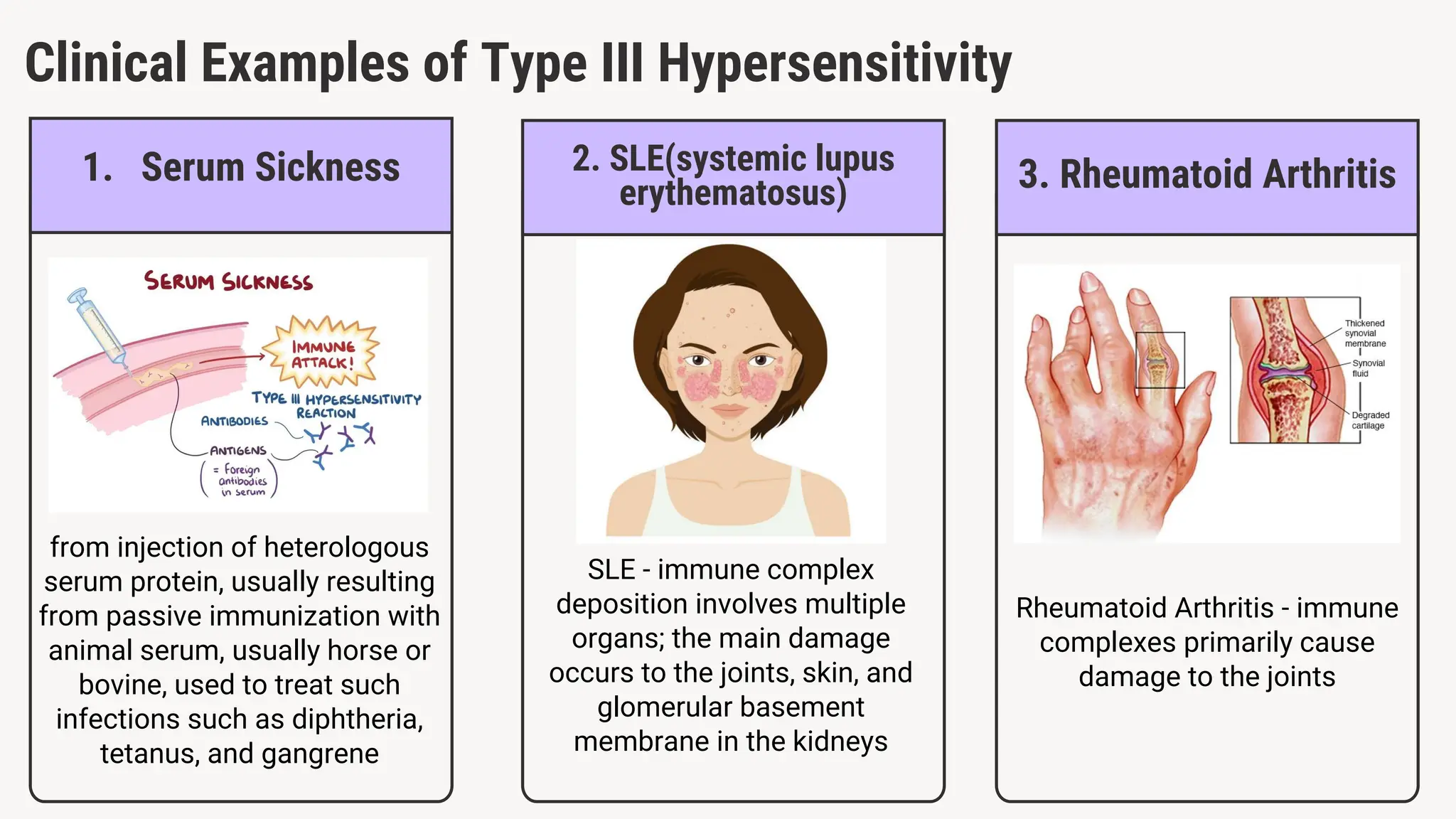
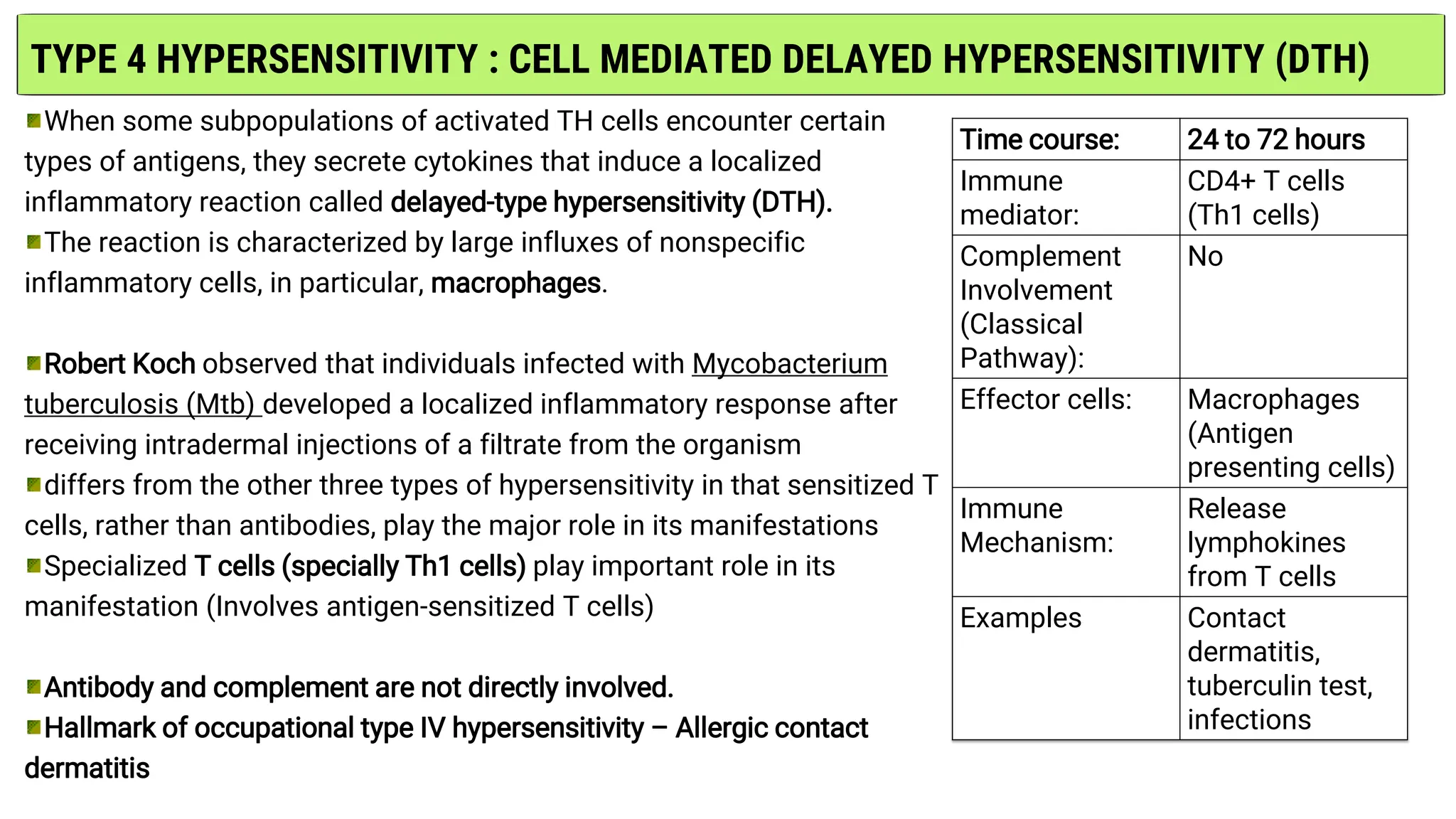
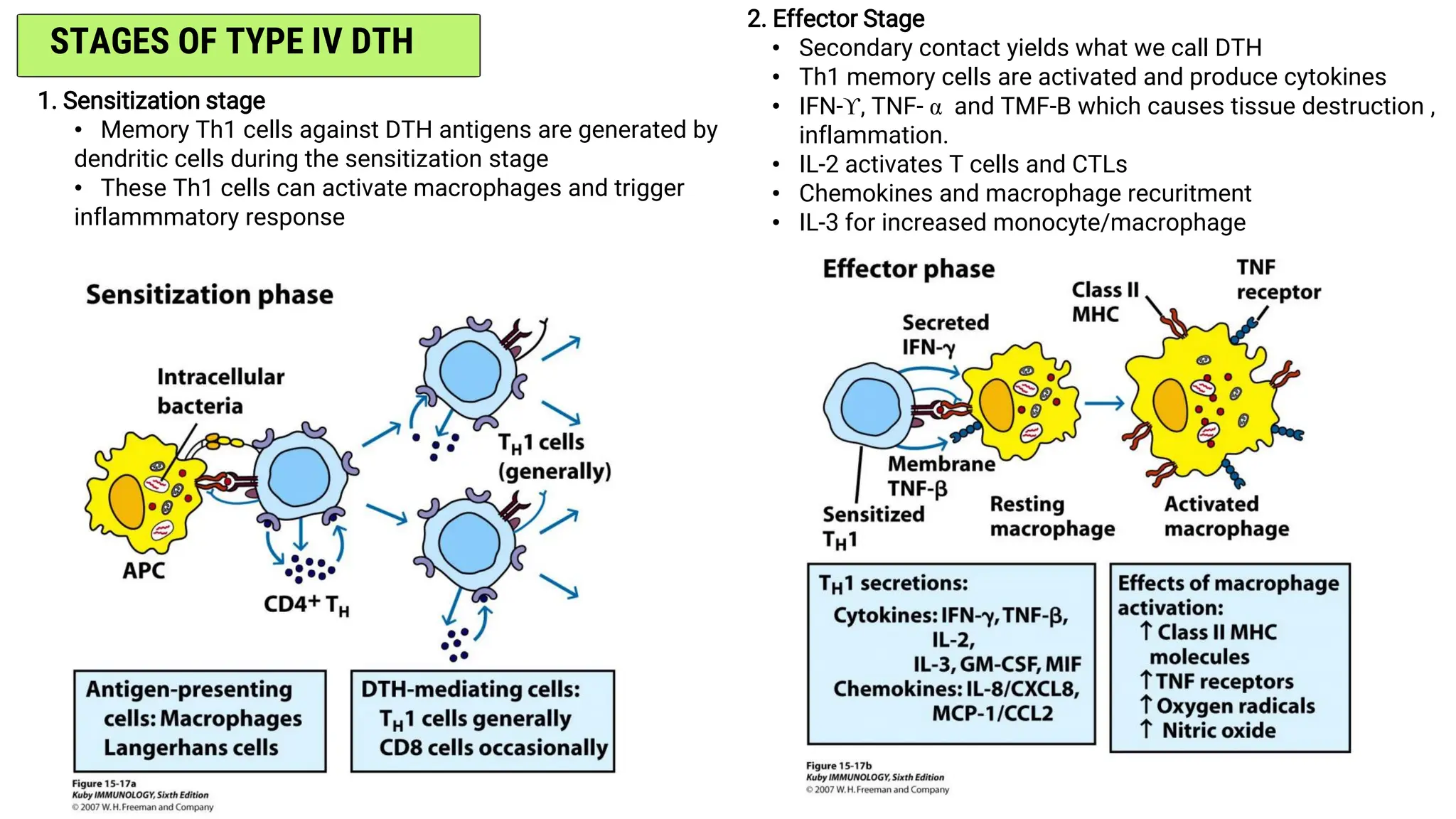
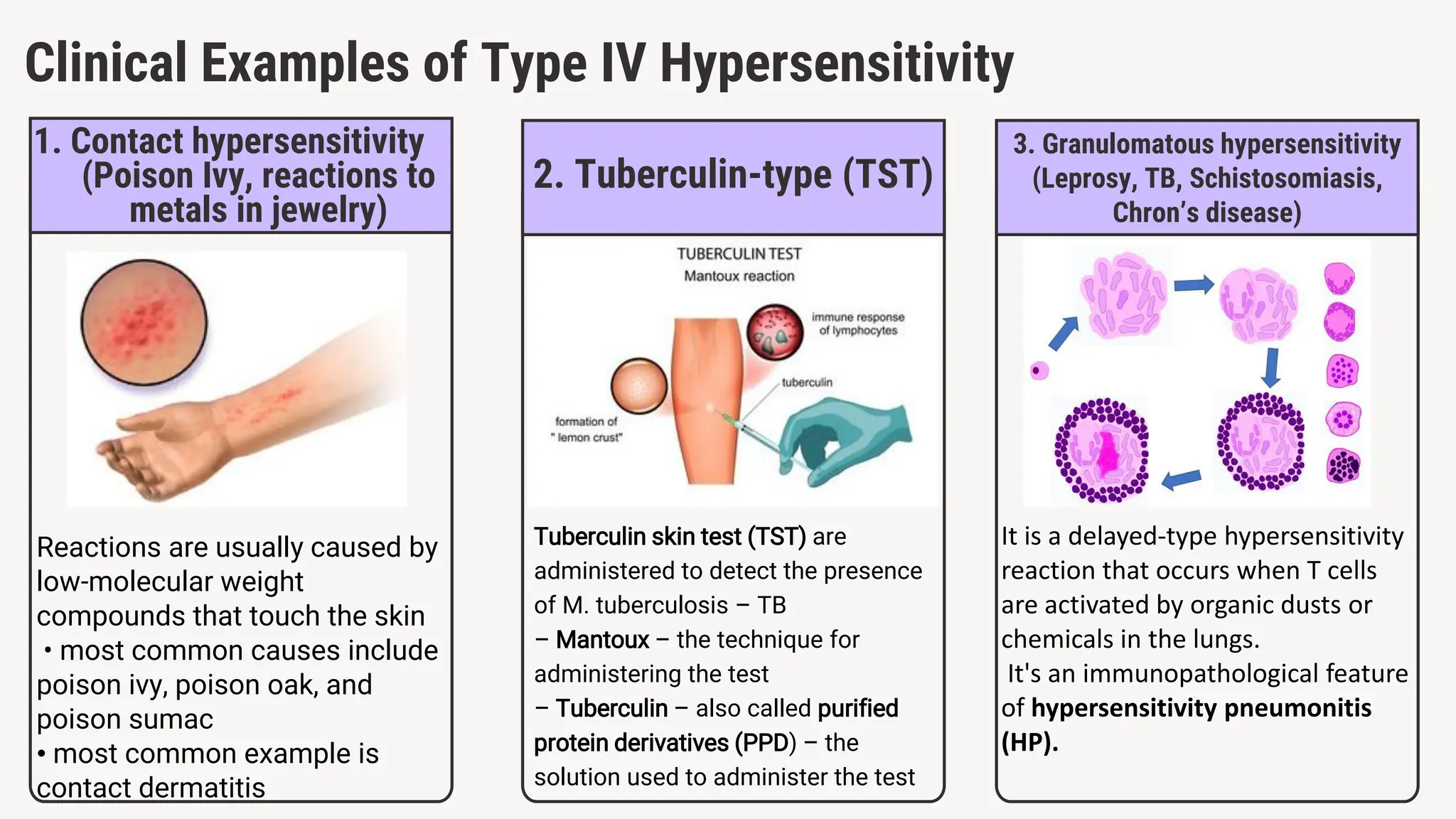
This presentation provides a comprehensive overview of hypersensitivity reactions, which are exaggerated or inappropriate immune responses to antigens. It explains the four types of hypersensitivity (Type I–IV), their mechanisms, clinical examples, and immunological basis. Special focus is given to conditions like allergies, autoimmune diseases, and transplant rejection, supported with diagrams and case studies to enhance understanding. Suitable for medical, biotechnology, and life sciences students.