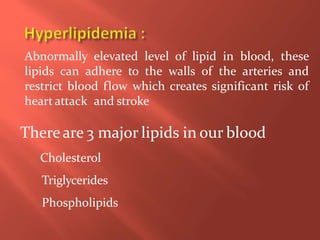
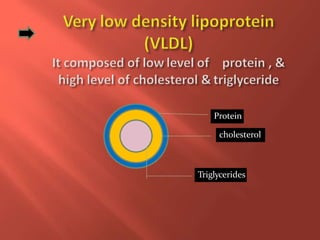
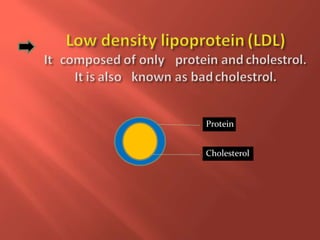
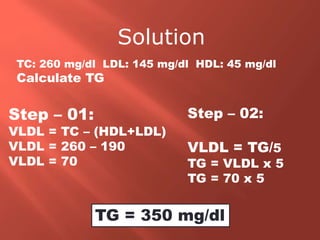
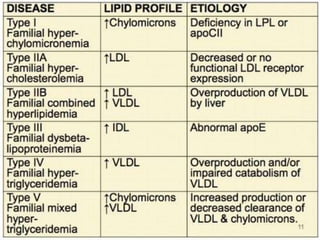
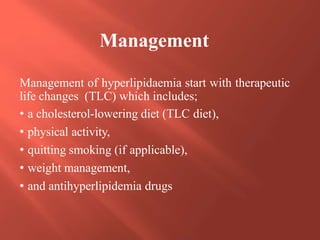
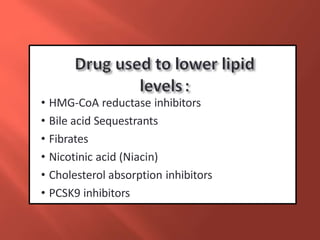
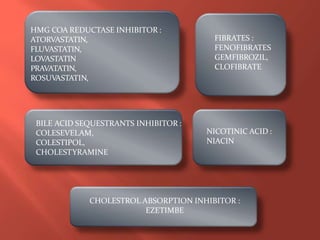
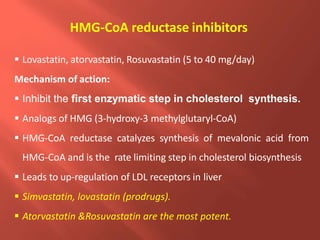
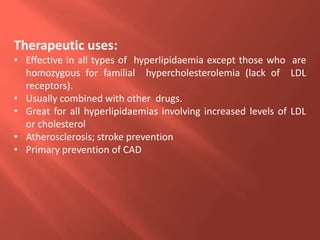
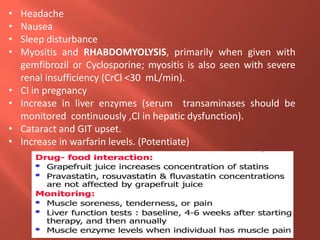
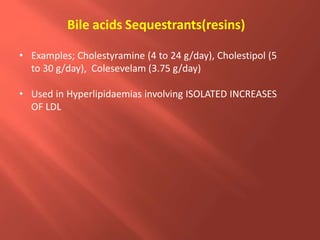
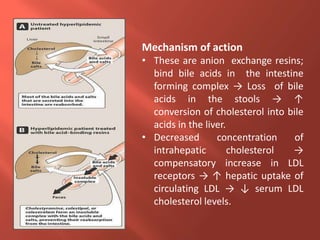
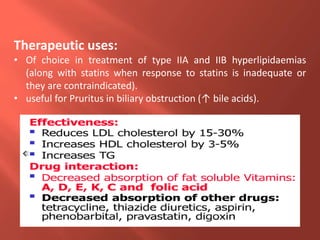
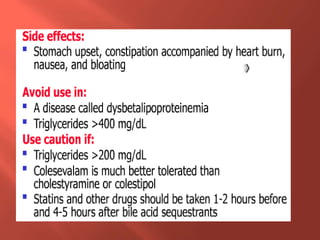
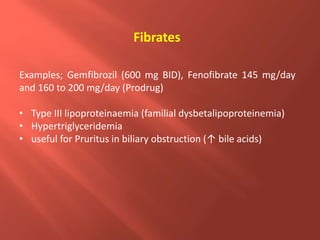
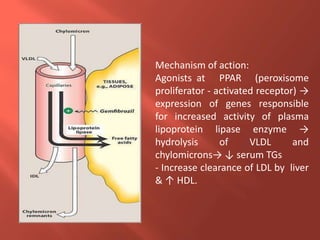
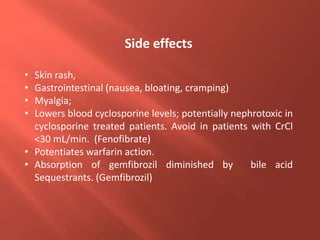
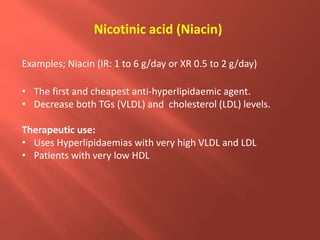
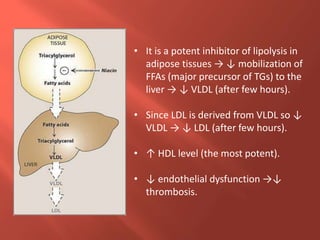
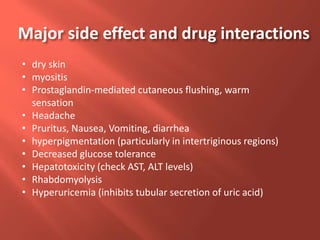
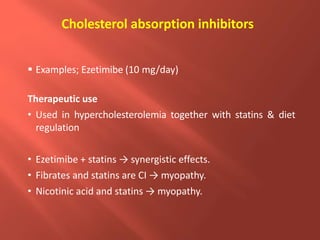
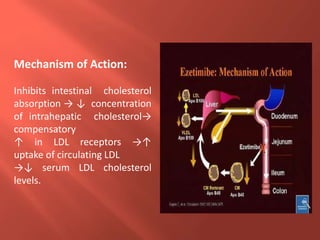
This document summarizes key aspects of lipid metabolism and hyperlipidemia management. It defines lipids and lipoproteins, describes their normal roles and abnormalities. Mechanisms and examples of different drug classes for treating hyperlipidemia are provided, including statins, fibrates, bile acid sequestrants, nicotinic acid, ezetimibe, and PCSK9 inhibitors. Their mechanisms, therapeutic uses, side effects and drug interactions are concisely outlined. Non-drug management including lifestyle changes and therapeutic lifestyle counseling are also mentioned.