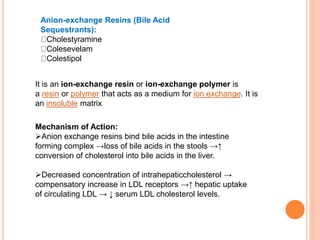
This document discusses drugs used to treat hyperlipidemia. It begins by defining different lipoproteins such as LDL, HDL, and VLDL. It then classifies anti-hyperlipidemic drugs into 5 main groups: statins, fibrates, bile acid sequestrants, nicotinic acid, and cholesterol absorption inhibitors. For each drug class, it describes the mechanism of action, pharmacokinetics, therapeutic uses, adverse effects, and drug interactions. It emphasizes that combination drug therapy can maximize lipid lowering effects while minimizing toxicity and achieving desired effects on various lipoproteins.