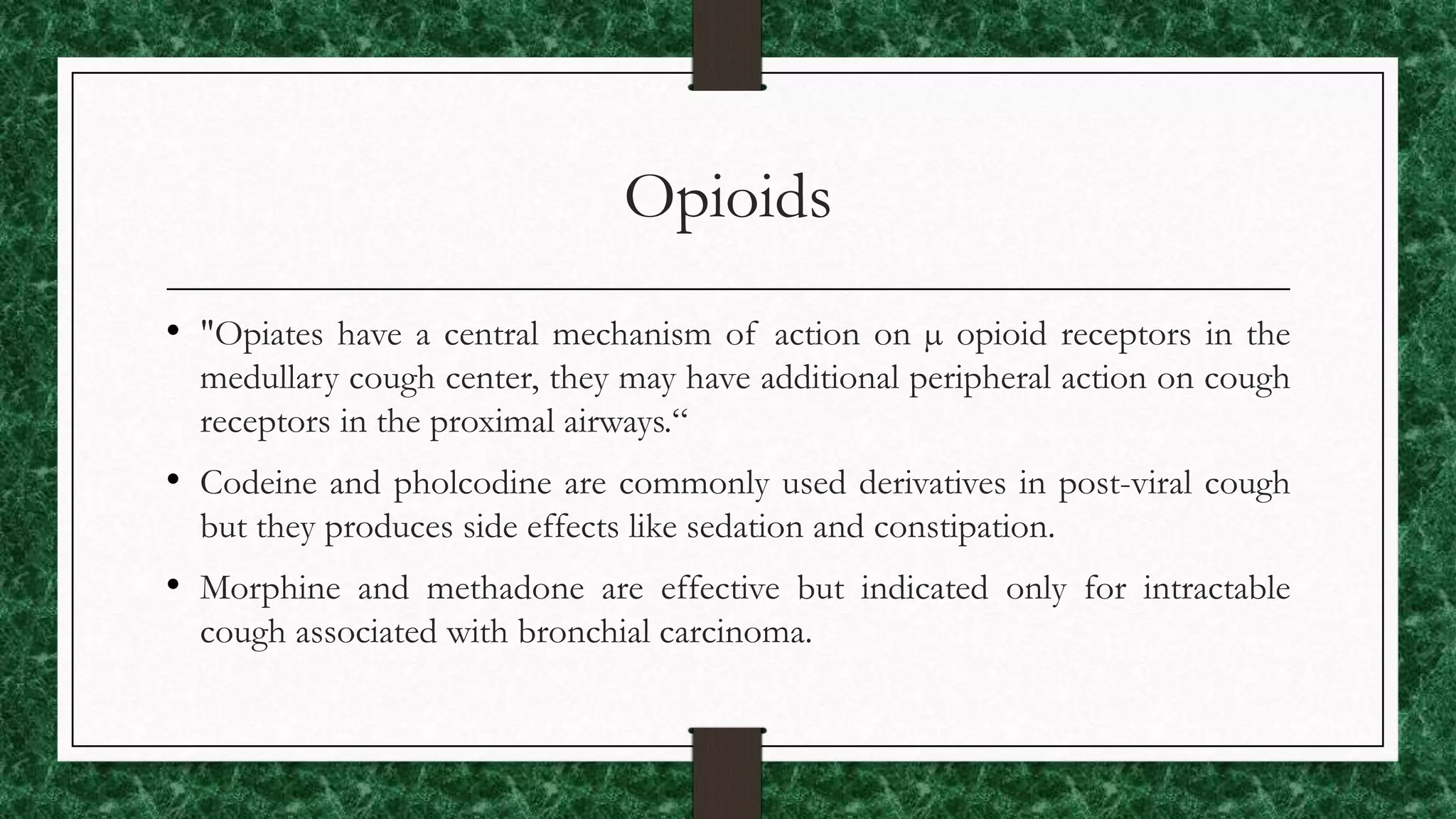
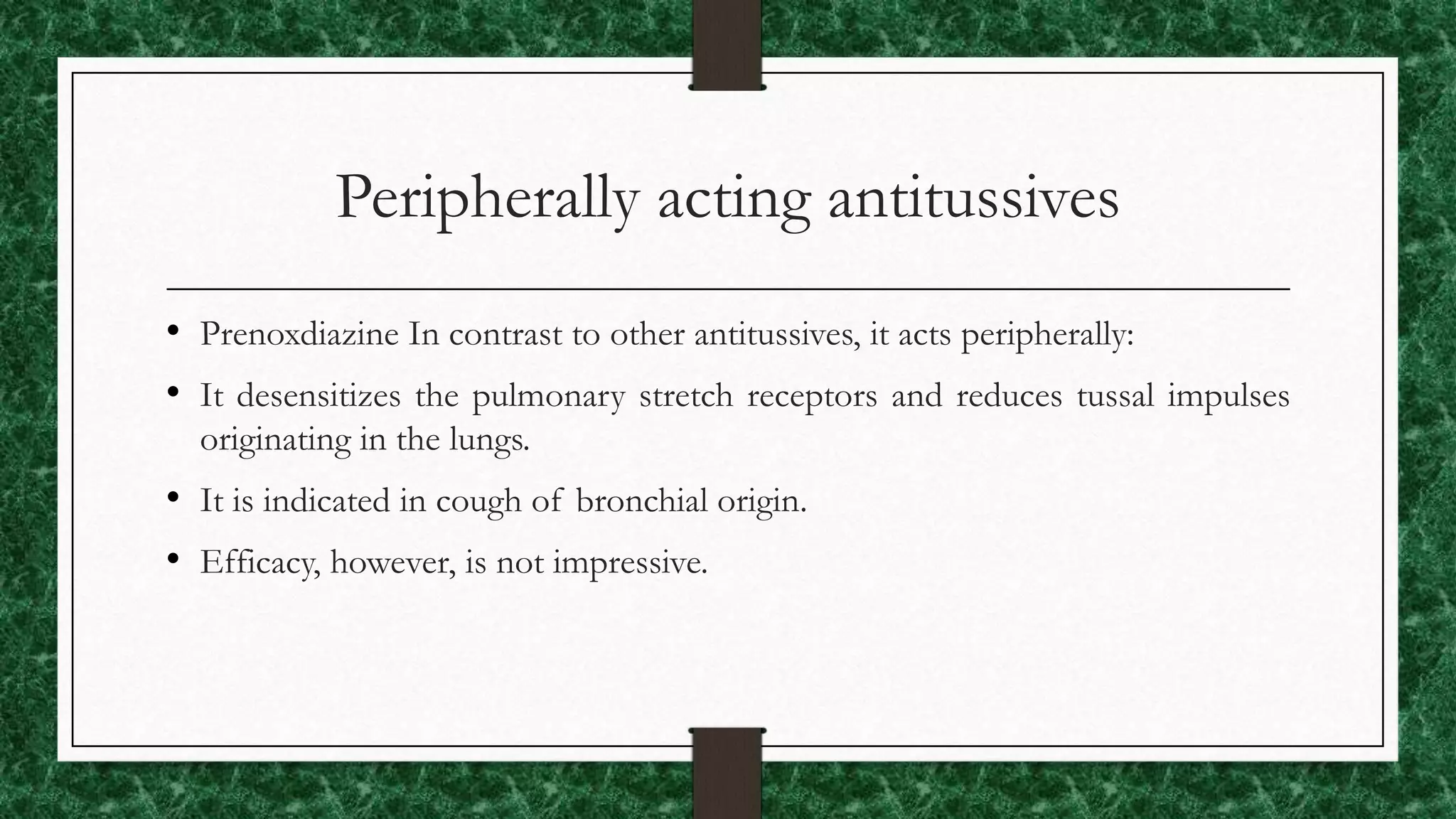
Expectorants are oral drugs that enhance bronchial secretion or reduce mucus viscosity to facilitate clearance by coughing, classified into bronchial secretion enhancers and mucolytics. Antitussives are drugs that raise the cough threshold in the CNS or act peripherally to reduce cough impulses, with classifications including opioids, non-opioids, antihistamines, and peripheral agents. Current treatment emphasizes caution in using antitussives for dry coughs, with a focus on identifying underlying causes and considering alternatives like hydration and steam inhalation.