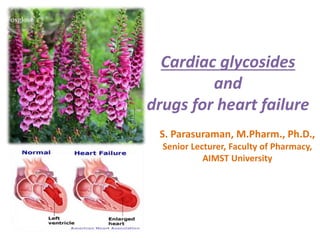
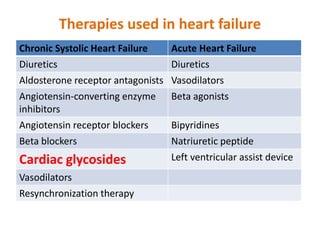
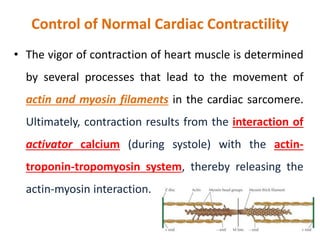
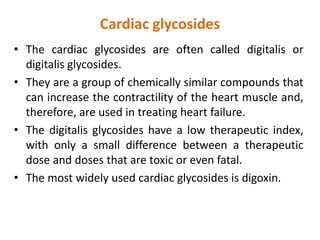
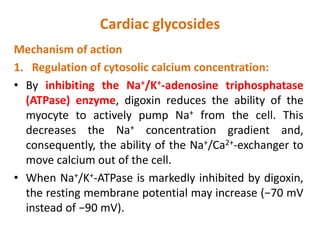
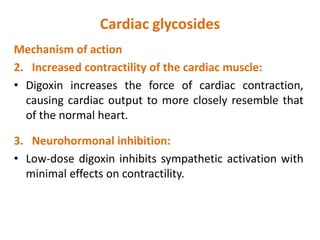
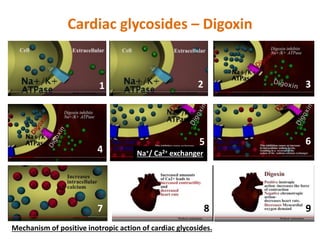
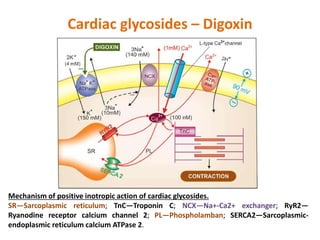
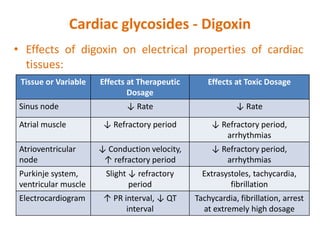
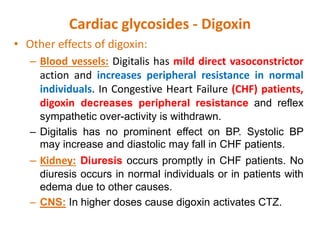
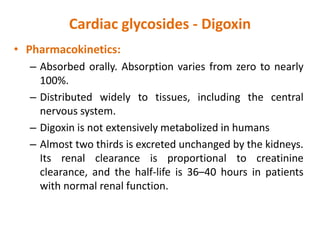
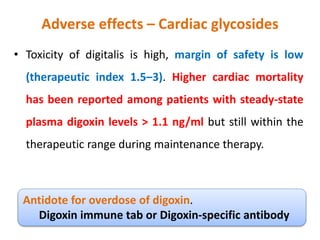
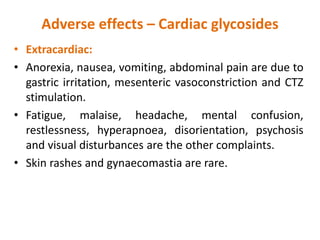
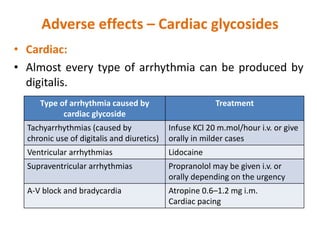
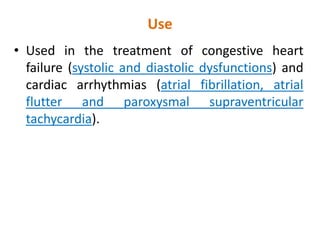
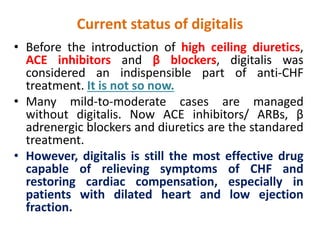
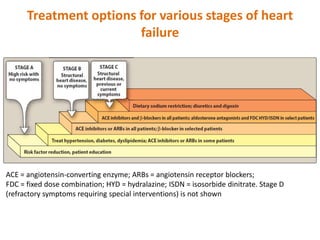
Cardiac glycosides like digoxin are used to treat heart failure and cardiac arrhythmias. They work by inhibiting sodium-potassium ATPase, increasing intracellular calcium levels, and enhancing cardiac contractility. Common side effects include nausea, arrhythmias, and toxicity at high levels. While they were once a standard treatment, newer heart failure drugs like ACE inhibitors, ARBs, beta blockers, and diuretics are now preferred due to their better safety profiles. Digitalis remains an option when symptoms are not adequately controlled by other treatments.