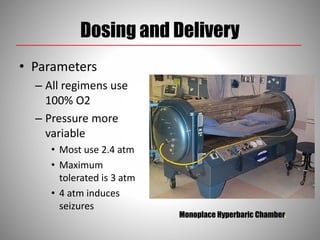
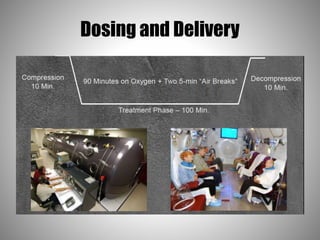
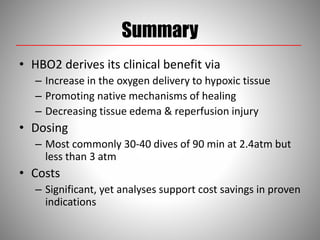
1. Hyperbaric oxygen therapy involves delivering 100% oxygen to a patient in a pressurized chamber at greater than 1 atmosphere to increase the amount of oxygen dissolved in the patient's plasma.
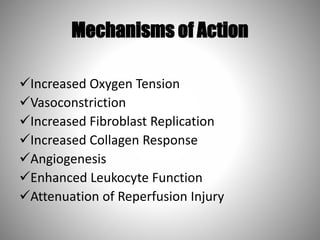
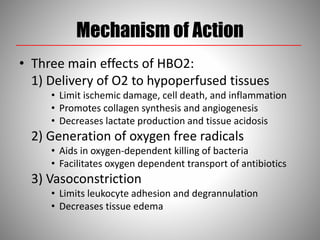
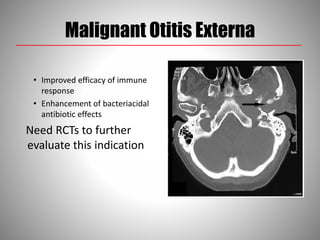
2. It has a variety of proposed mechanisms of action including increasing oxygen delivery to tissues, generating oxygen free radicals to aid in bacterial killing, and causing vasoconstriction.
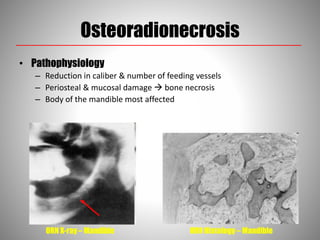
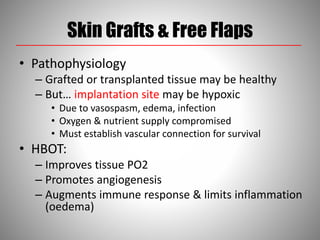
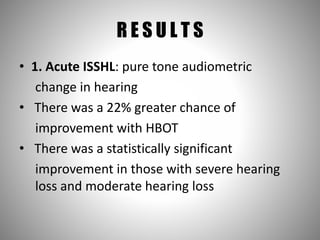
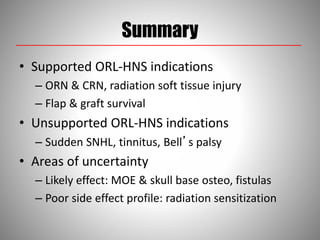
3. It has been used to treat conditions like problematic wounds, radiation injury, decompression sickness, and sudden hearing loss. The evidence for its use is strongest for problematic wounds and enhancing graft and flap viability after surgery.