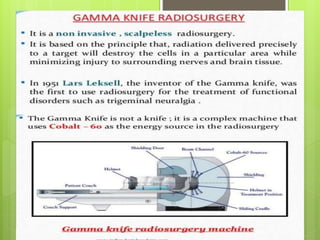
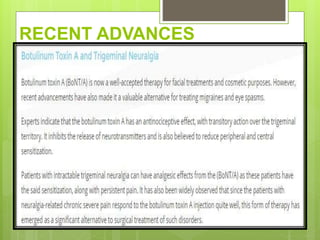
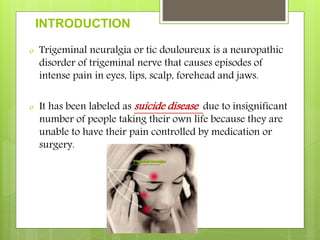
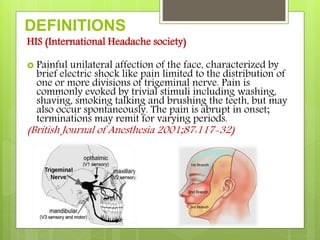
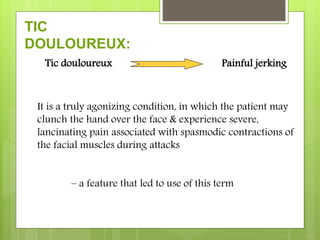
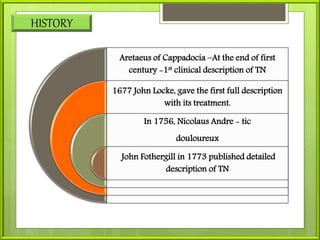
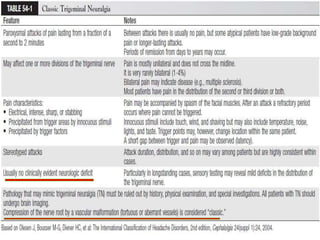
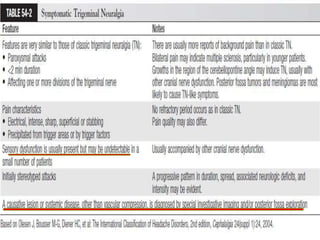
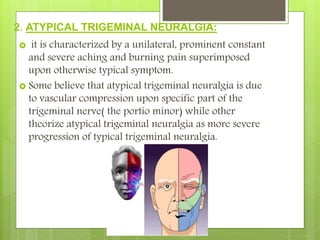
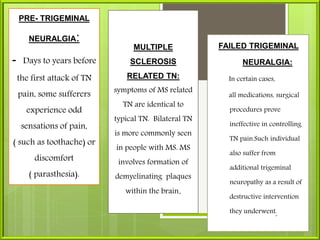
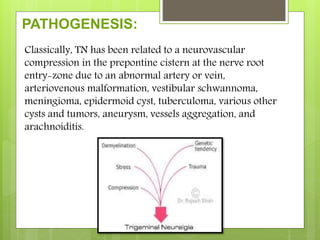
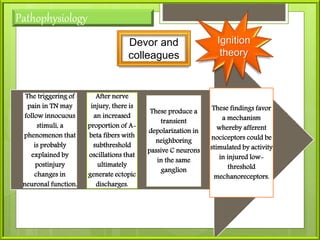
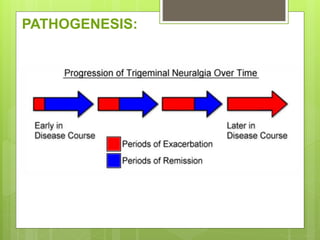
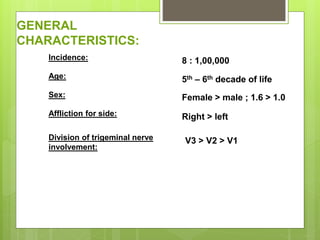
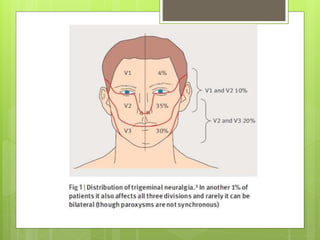
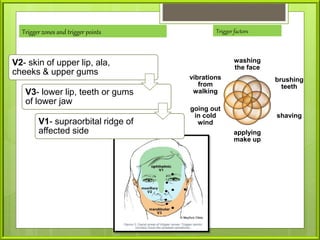
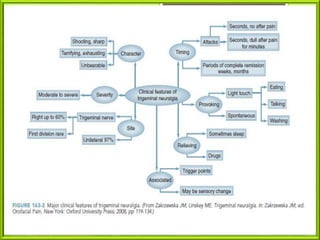
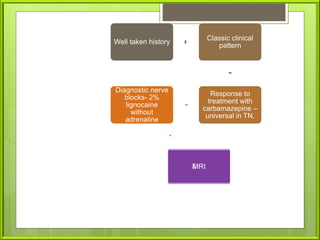
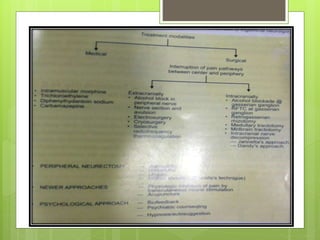
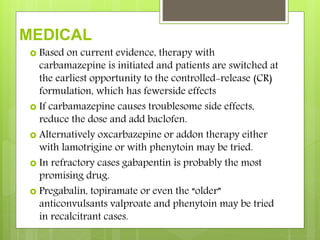
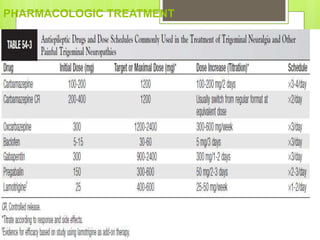
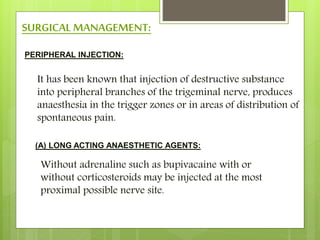
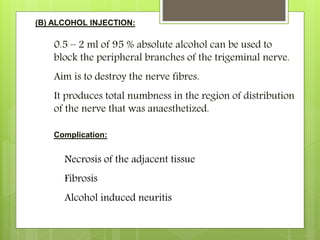
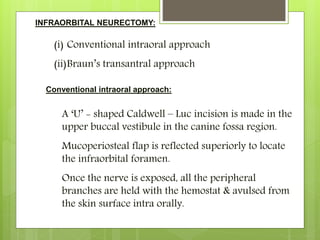
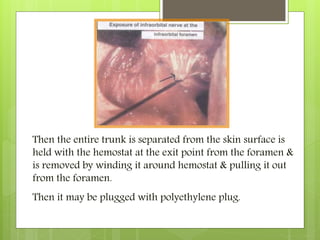
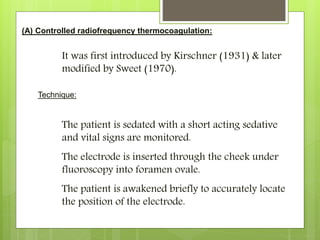
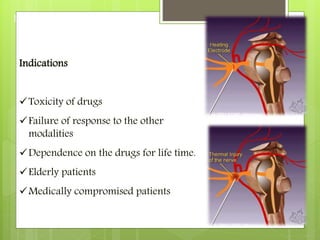
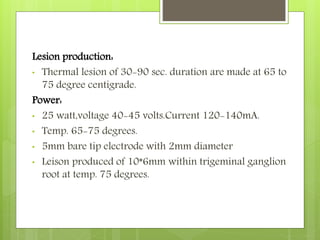
The document provides an overview of neuralgia, specifically trigeminal neuralgia. It begins with definitions of trigeminal neuralgia and discusses its historical understanding. Trigeminal neuralgia is classified and its etiology, pathogenesis, general characteristics, and clinical characteristics are described. The diagnosis of trigeminal neuralgia involves clinical examination and diagnostic tests. Treatment options include pharmacological treatments primarily using carbamazepine as well as surgical treatments targeting peripheral nerves or central ganglia. Recent advances in understanding the condition are also mentioned.

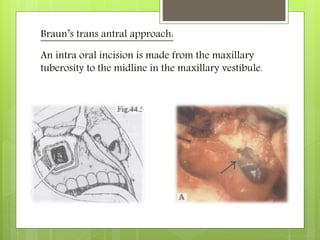
![NEURALGIA
Presented by:
Sarin A.Nizar
[PG/Oral and Maxillofacial Surgery]](https://image.slidesharecdn.com/tnfinalsarin-160420160057/85/trigeminal-neuralgia-2-320.jpg)
![CLASSSIFICATION
ATYPICAL TN
TYPICAL TN
TN
IDIOPATHIC/PRIMARY SECONDARY
ACCORDING TO DANTY[1934]
TN HAS BEEN CLASSIFIED AS
CLASSIC TRU
E](https://image.slidesharecdn.com/tnfinalsarin-160420160057/85/trigeminal-neuralgia-10-320.jpg)


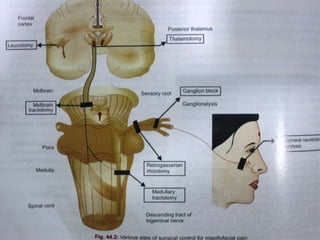
![(B) Trigeminal root section:
(a) Extradural sensory root section:Frazier Approach[1901]
It is also known as the subtemporal extradural
retrogasserian rhizotomy.
It is no longer used now.
In this, sensory root is divided, sparing the motor
root, as close to the brainstem as possible.
Disadvantage:
Profound sensory loss
High incidence of anaesthesia dolorosa](https://image.slidesharecdn.com/tnfinalsarin-160420160057/85/trigeminal-neuralgia-71-320.jpg)
![(b) Intradural rhizotomy:
Described by Wilkins[1966]
This is an intradural procedure that is done when
the pain recurs after MVD.
This is usually done in the posterior cranial fossa.
It can be selective or complete.
(c) Trigeminal tractotomy:
It is also known as the medullary tractotomy.
This is not usually done.
The descending tract of the trigeminal nerve is
sectioned at the junction of the cervicomedullary
region.](https://image.slidesharecdn.com/tnfinalsarin-160420160057/85/trigeminal-neuralgia-72-320.jpg)