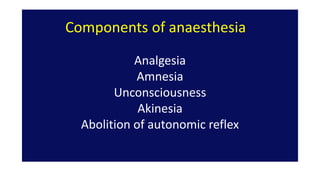
The document discusses induction, maintenance, and reversal of anesthesia. It describes:
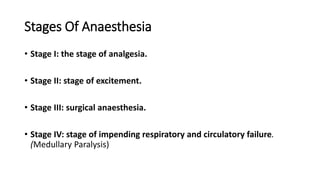
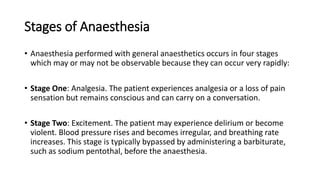
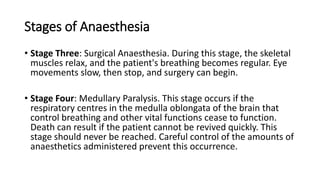
- The 4 stages of anesthesia from analgesia to medullary paralysis
- Common methods of induction including intravenous and inhalational agents
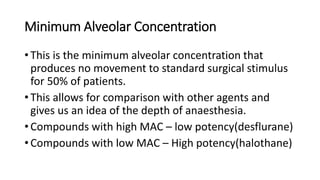
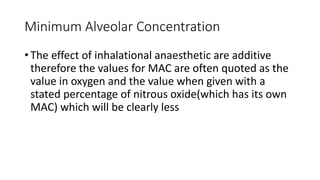
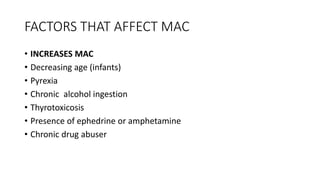
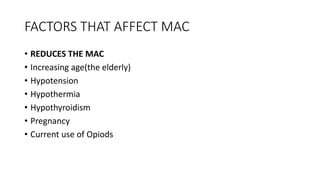
- Factors that determine the minimum alveolar concentration of inhalational anesthetics
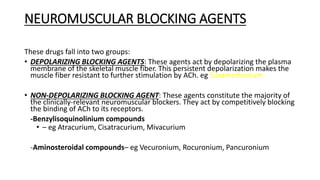
- Use of muscle relaxants during induction and maintenance
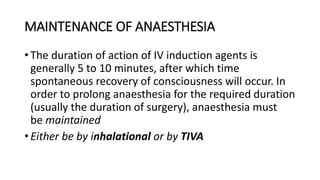
- Techniques for maintenance including inhalational and total intravenous anesthesia
- Reversal of muscle relaxation using anticholinesterase drugs and assessing neuromuscular blockade.