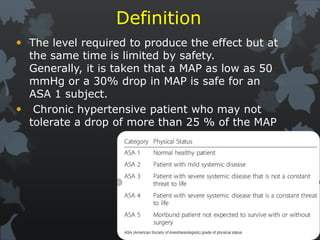
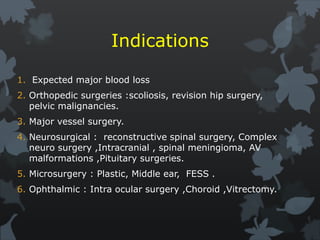
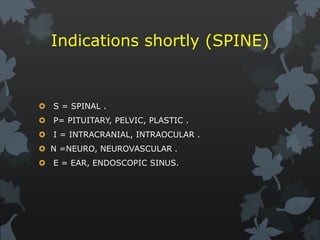
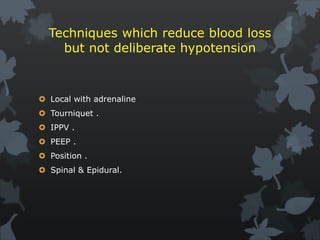
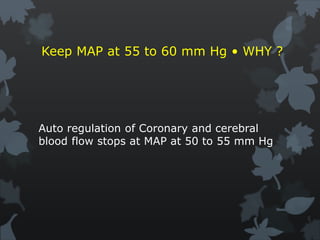
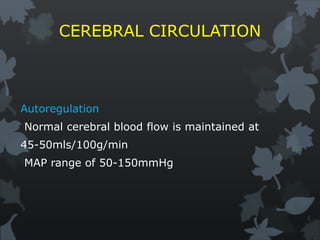
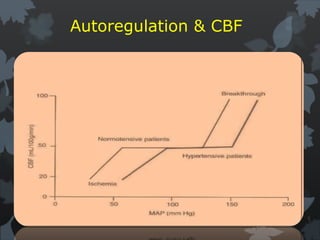
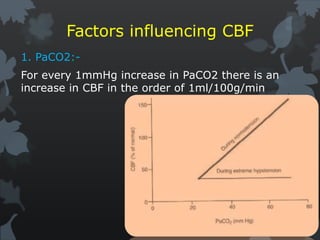
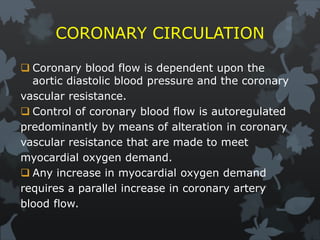
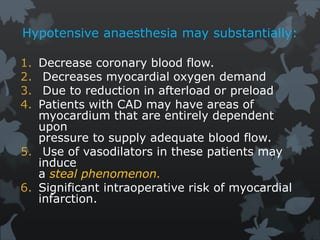
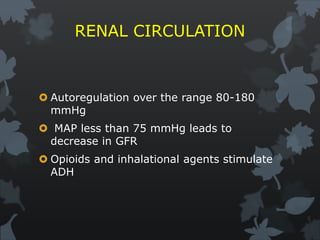
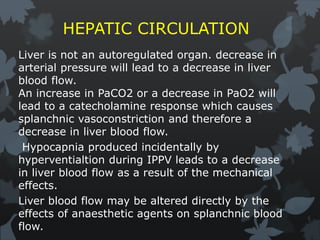
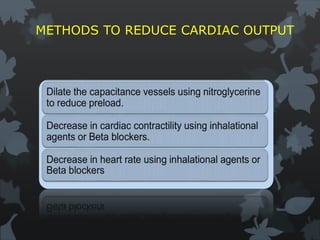
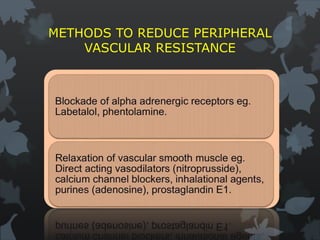
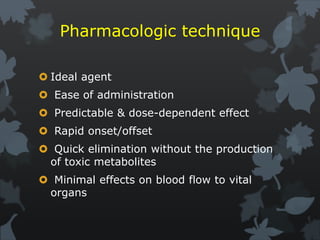
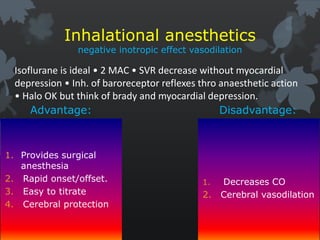
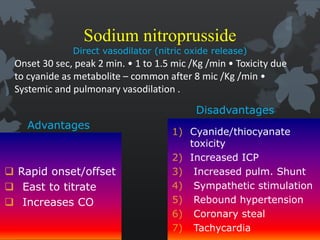
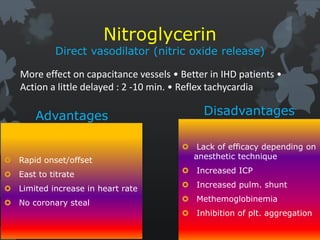
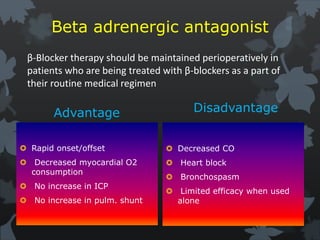
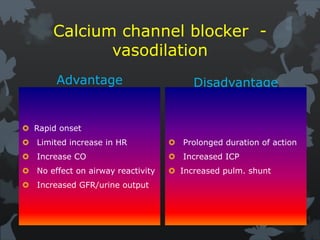
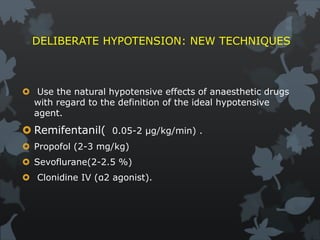
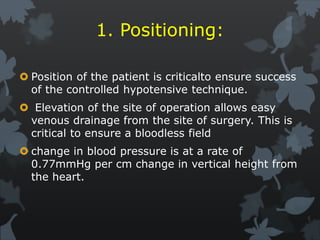
This document discusses hypotensive anesthesia techniques. It begins with the aims of deliberate hypotension during surgery, which are to provide an adequate surgical field, decrease blood loss in vascular areas, and avoid the need for blood transfusions. It then covers the physiology of blood flow regulation in vital organs like the brain, heart, kidneys, and liver that must be considered. Various pharmacological agents and mechanical techniques for reducing blood pressure are outlined. Strict patient selection, monitoring, fluid management and postoperative care are emphasized for safely using hypotensive anesthesia.