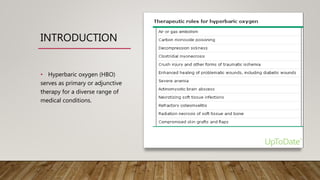
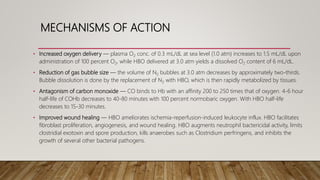
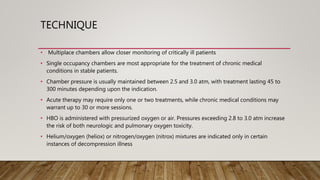
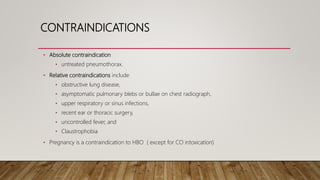
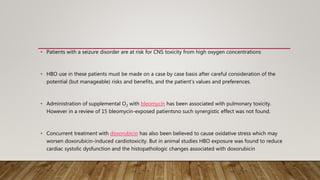
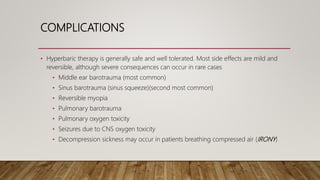
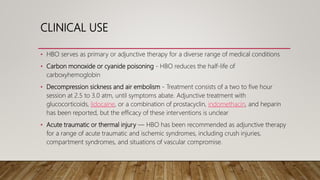
This document discusses the current role of hyperbaric oxygen therapy (HBOT). It begins by explaining the mechanisms of HBOT, including how it increases oxygen delivery to tissues and reduces gas bubble size. It then describes the techniques used, including chamber pressures and treatment durations. The document outlines the contraindications and complications of HBOT. It concludes by describing the clinical uses of HBOT for conditions like carbon monoxide poisoning, decompression sickness, traumatic injuries, radiation injury, infections, and non-healing wounds.