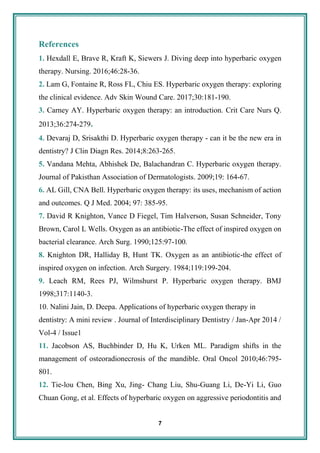
1. Hyperbaric oxygen therapy (HBOT) involves breathing pure oxygen in a pressurized chamber, which increases the amount of oxygen that dissolves in the patient's plasma and tissues. This promotes healing and reduces recovery time.
2. HBOT works by increasing oxygen tension in tissues through several physiological effects, including increased angiogenesis and fibroblast proliferation. The increased oxygen aids neutrophils in fighting infection and promotes tissue regrowth.
3. HBOT is used to treat osteoradionecrosis, refractory osteomyelitis, and compromised bone healing after radiation therapy for dental implants through its effects on increasing oxygen delivery and stimulating cell growth in hypoxic tissues.